Abstract: This article analyzes the impact of the coronavirus epidemic in India after first situating it in the wider international context. It begins with a global perspective on the spread of the pandemic that correlates more with geography, demography and seasonality than lockdown stringency and sequencing. The responses of governments have damaged economies, lost livelihoods, worsened healthcare-access and learning-outcomes, while curbing rights and freedoms of citizens. In India, the draconian lockdown dealt a crippling blow to the economy which has hurt the poor badly but could not ‘flatten the curve’. The inadequate and inappropriate policy response has made the task of economic recovery even more difficult. Yet, the crisis also opens possible opportunities for India to enhance its global role and profile.
Keywords: Covid-19, India, lockdowns, lives, livelihoods, economic contraction, unemployment, immunities, liberties.
A novel coronavirus emerged from the wet markets of Wuhan China in late 2019 by hopping across from animals to humans. Initially endorsing Chinese official claims that there was no evidence of human-human transmission, it wasn’t until 11 March 2020 that the World Health Organization (WHO) declared a pandemic. The rest of the world at first thought this was a local problem for China, and then was shocked at the brutality of the lockdown clamped on Wuhan by the authorities to quarantine the infection cluster. But soon the virus caught the highways and byways of globalization to quickly encircle the world. Other countries realized their hospital systems could be overwhelmed unless they flattened the curve of the virus to drastically slow down the surge of new infections. In particular, no country had the requisite number of beds in its intensive care units (ICUs) to manage patient loads under worst-case scenarios. At this point China’s response began to be reinterpreted as brutally effective, not just brutal, and perhaps worthy of emulation because of its demonstrable success. This despite the fact that China’s claimed success based on official figures is highly implausible, as Sebastian Rushworth, a practising physician in a Stockholm hospital, points out in one of his excellent blog posts (3 January).
The virus response spectrum has spanned four possible policy approaches: “let it rip” do nothing; flatten the curve; community suppression that aims to stop person-person transmission within a territorially demarcated community; and elimination. Belarus, Nicaragua and Tanzania may have gotten away with the first, but no serious expert recommends it. Elimination is not possible either, as it would require local, national and global eradication. Like other respiratory infections, coronaviruses keep circulating, albeit with progressively decreasing virulence in subsequent waves as part of the natural evolution of the virus curve. In an average year, around 3mn people die of flu and pneumonia in the world despite the availability of vaccines. Similarly, it is extremely unlikely we will ever get to a zero level of Covid risk. Instead, the key question is to decide on the level we are willing to accept relative to the damage done to society and the economy by mitigation strategies. This is ultimately a political question, not one to be decided by health bureaucrats and doctors. Dr. Mike Ryan, head of the WHO Emergencies Programme, at the year’s final press conference on 28 December, said Covid-19 is likely to become endemic in the global population. Vaccinations do not guarantee that infectious diseases will be eradicated. Instead, societies would do better to focus on getting back to full strength, rather than on the “moonshot of eradication.”
Consequently, the responses of most governments divide between the second and third options. Social distancing is intended only to contain infection transmission, not suppress infections and related fatalities. At some stage, however, many countries seemed to quietly switch from flattening the curve to protect the health system, to the more ambitious strategy of community suppression, which had the perverse if unintended effect of slowing the attainment of herd immunity; and even, as in the case of New Zealand, move toward eradication by closing off the country until an effective vaccine was available and acting aggressively to suppress any outbreak of infection in the community until then.
While this was successfully done in the case of smallpox, with a virus it may be a dangerously delusional ambition. In the early 1950s, an estimated 50mn cases of smallpox occurred in the world each year, millions of whom died. Thanks to WHO’s initiative and efforts, it was eradicated by 1980 after an eleven-year effort at a total cost of around $300mn. Governments and people may be over-estimating the impact of the Covid-19 vaccines. Based on early reports, the Covid-19 vaccines approved for mass manufacture will help to reduce the severity of symptoms but may not save lives, guarantee immunity to infection or prevent transmission. Their efficacy for subgroups, especially the elderly, is unknown, as is their short and long-term side effects.
“Herd immunity” – where “the chain of contagiousness toward the vulnerable” is broken when enough of the population has acquired immunity to an infection – is very controversial. An important part of the explanation for the public distaste concerning the concept of herd immunity lies in scientists’ remoteness from the public relations nuances of a technical term that they, the scientists, understand to be value neutral. To the general public it carries connotations of relegating human beings to the status of cattle. We will substitute “population immunity” to mean the same. The pharmaceutical intervention route to population immunity is through vaccines which is common and uncontroversial. Indeed, typically it is the ‘anti-vaxxers’ (people opposed to vaccinations) who are derided as science deniers. The natural route to population immunity is through T-cell-based immunity and antibodies that could permit a gradual but controlled spread of the virus without overwhelming the health system. The reason most governments shied away from the herd strategy was the assumption that this requires two-thirds of the population to be infected. With the initial alarming fatality rates reported from China, the horrific scale of lives this would have sacrificed was unacceptable.
However, more recently researchers have begun to suggest that the immunity threshold could be much lower because fatality rates are lower than initially projected by the fear-generating models. Major news media – Guardian, BBC, New York Times – have finally begun to take note. One team looked at human genomic datasets for possible explanations for the strikingly lower rates of Covid-19 infections and mortality in East Asia that has been the geographic origin of several modern coronavirus epidemics. Their results, published on 16 November 2020, suggest that ancient coronavirus-like epidemics drove adaptations in East Asia between 25,000-5,000 years ago.
We believe, but do not develop the argument here, that the fate of this virus is going to be determined by two variables: what fraction of the population acquires immunity through vaccination and infection, including asymptomatic infection; and what proportion of the population already has some form of resistance to it. Thus, in our view, all governments should respond to coronavirus with effective risk management, instead of reacting in panicked haste with misconceived policies. With respect to India, we argue that saving lives and preserving livelihoods are symbiotically entwined. Together they shape the wellbeing of people and it is for the government to reconcile these objectives instead of letting it be posed as a false either-or choice. We further argue that the draconian and prolonged lockdown dealt a crippling blow to the Indian economy and placed a disproportionate burden on the poor, while the grossly inadequate response of the government to mitigate the harsh impacts on the people and the economy has made the task of post-pandemic recovery even more difficult.
The Global Context
The focus of this article is on India. Before discussing India, however, it is useful to summarize the global context of Covid-19 with eight observations.
First, the geographic spread of the virus has been strikingly uneven among continents (Figure 1) and even within them. Oceania and Africa were the most lightly affected. Australia and South Africa, the worst hit in the two regions respectively, have just 35 and 489 deaths per million people (DPM, figures as of 3 January 2021). Only 7 of the 57 African countries have a mortality rate of over 100 DPM. Western Europe and the Americas were the most severely impacted. The chart, following UN regional groupings, includes Central Asia and the Middle East in Asia, which distorts the latter’s overall statistics. For example, eight countries (Armenia, Georgia, Iran, Iraq, Israel, Jordan, Oman, Palestine) have on average 516 DPM. In Asia minus the Middle East, India and the Philippines suffered the most, but still with lowly 108 and 84 against the world average of 236 DPM. Even on its own, before looking at the impact of lockdown measures, this already indicates the folly of generalizing across countries and continents. Instead, it is better to look at the specific circumstances of each country. In Oceania, Australia’s low toll, for example, might be better explained by its geographical location, physical isolation, vast open spaces, low density living, few multigenerational households, high use of private cars instead of mass transit, and sociocultural practices.
Second, the cascading lockdown measures imposed across Europe and the Americas were a radical, even experimental, departure from the existing orthodoxy. Until 2020, the official WHO position was contained in an 85-page report in October 2019. It provided recommendations for the use of non-pharmaceutical interventions (NPIs) in future influenza epidemics and pandemics “based on existing guidance documents and the latest scientific literature.” NPIs recommended for dealing with pandemics included hand hygiene, respiratory etiquette (such as covering coughs and sneezes, using tissues and then throwing them away), face masks for symptomatic individuals, surface and object cleaning, increased ventilation, isolation of sick individuals, travel advice, avoidance of crowding, and, for a pandemic of exceptional severity, workplace measures and closures and internal travel restrictions. By contrast, border screenings and closures, entry and exit screenings, quarantine of exposed individuals, and contact tracing (and, for epidemics, even internal travel restrictions), were not recommended in any circumstances (p. 3, Table 1).
There were two reasons for the scepticism. For one, “sufficient evidence” exists to show ineffectiveness of entry and exit screening; and “weak evidence” that travel restrictions may delay the introduction of infections only temporarily and can adversely affect mitigation programs and disrupt supply chains, while border closures may work for small island nations in severe cases “but must be weighed against potentially serious economic consequences.” For another, “social distancing measures… can be highly disruptive, and the cost of these measures must be weighed against their potential impact.” The 2019 WHO consensus report was foreshadowed in a 2006 study by a team led by Thomas Inglesby, Director of Johns Hopkins’ Bloomberg School of Public Health. The final paragraph of that paper concluded with this “overriding principle”: “Experience has shown that communities faced with epidemics… respond best and with the least anxiety when the normal social functioning of the community is least disrupted.”
What happened to overturn the existing consensus? It was certainly not new science. There simply was no time to conduct rigorous new studies following standard procedures, randomized clinical trials and peer reviewed publications on the emergence, growth, curve, and retreat of the virus, let alone the best mitigation and suppression measures to fight it. Mortality rate is the frequency of deaths within a time period relative to the size of a well-defined population: DPM is a standard metric. An infection fatality rate (IFR) is defined as the proportion of deaths relative to the prevalence of infections within a population. IFRs from samples across the population include undiagnosed, asymptomatic, and mild infections. A case fatality rate (CFR), based exclusively on relatively smaller groups of moderately to severely ill diagnosed cases at the beginning of an outbreak, is defined as the proportion of deaths among confirmed cases of the disease. In the US, says Dr Ronald Brown in a peer-reviewed article, “due to misclassifying an IFR as a CFR, the comparison turned out to be between an adjusted coronavirus CFR of 1% and an influenza IFR of 0.1%.” Not surprisingly, the prospect of a new disease ten times as deadly as the average flu was alarming and led to a cascade of disproportionate responses.
This begs the question: have the peoples of the world been subjected to an unethical experiment in contravention of the science? Before implementing mitigation measures that incur severe costs, the onus is on proponents to formally reject the null hypothesis by justifying claims of life-saving benefits. Yet lockdowns and other mitigation measures were implemented with minimal supporting evidence. For example, Abiel Sebhatu et al. concluded that OECD countries essentially mimicked one another’s Covid-19 restrictive policies: a clear demonstration of herd behaviour by governments. Either the WHO guidance was not based in science and the epidemiologists have access to better scientific knowledge, in which case the public needs to know the basis of their confidence over that of the existing WHO advice at the start of the pandemic. Or else the existing science behind the 2019 advice was sound, in which case the closures privileged abstract mathematical modelling over actual science based on observational data and medical scholarship.
Third, rather than scientific consensus, there’s considerable uncertainty. The coronavirus science has been unsettled and vigorously contested regarding infectiousness, lethality, transmissibility, and the effectiveness of various forms of preventive practices, NPIs and pharmaceutical interventions. Should schools be closed? Should masks be universally mandated? Should ivermectin and hydroxychloroquine be prescribed or prohibited to treat the disease? Perhaps most critically, should the overriding strategy be to do nothing, or to aim for flattening the curve, stop community transmission, or eradicate the virus? In these circumstances, reasoned discussion of all options should be welcomed and facilitated. As a thoughtful letter to the British Medical Journal on 21 September from Raj Bhopal, emeritus professor of public health at Edinburgh University, put it, silencing and removing sceptical and contrarian voices from the public space “is irresponsible at this time of global crisis.”
To take but one example, the science on face masks can be looked at for cloth/gauze versus medical/surgical masks, healthcare workers and general populations, open spaces and closed settings, sick and healthy people, and laboratory experiments and randomized controlled trials. In communitarian-minded East Asia, non-surgical masks are mostly used by the sick to avoid infecting others, not by the healthy as a prophylactic. Oxford University’s Centre for Evidence-Based Medicine notes that “despite two decades of pandemic preparedness, there is considerable uncertainty as to the value of wearing masks.” Dr Andrea Ammon, Director of the European Centre for Disease Prevention and Control, holds that wearing masks has limited utility in restricting the spread of coronavirus, on the one hand, and could pose a potential health hazard, on the other, if it leads to complacency where people think it protects them enough to ignore personal hygiene and physical distancing.
Data from the Centers for Disease Control and Prevention (CDC) showed 71% of Americans “always” and 14% “often” wore a mask in the fortnight before the onset of Covid illness. The CDC evidence is powerfully buttressed by observational data showing that in country after country and in US states, caseloads surged in autumn despite universal mask mandates – and did not surge as sharply in Denmark, Norway and Sweden, which did not mandate masks. A large Danish study in the Annals of Internal Medicine reconfirmed that masks do not protect healthy people from being infected, as attested to earlier in the year by both the WHO and the CDC in the US. According to an article in the New England Journal of Medicine in May 2020, wearing masks “outside health care facilities offers little, if any, protection from infection… In many cases, the desire for widespread masking is a reflexive reaction to anxiety over the pandemic.”
Scientists disagree over the reliability of tests for determining Covid cases. There is not even an agreed methodology for counting Covid-19 deaths, producing variable reliability of statistics from different countries that are not always measuring the same thing. A readjustment of the official methodology in the UK revised the total death downwards by a substantial 10% in August. In Italy, one study estimated that only 12% of attributed deaths were caused by Covid-19. The CDC estimated that until 30 December, only 6% of all US deaths recorded as involving Covid-19 was of people without any existing comorbidity. For the other 94%, “on average, there were 2.9 additional conditions or causes per death.” In Australia, Epidemiology Report 22 recorded only 9% with no comorbidity in hospital admissions for the fortnight ending 2 August. This adds grist to the controversy mill over dying of or with Covid. Thus, we do not know if the vast majority or tiny fraction of ‘Covid’ deaths are from the virus. The impossible distinction distracts from a deeper reality. Across all age groups, the ‘marginal’ risk of death caused by Covid is small (see the age-segregated survival rates from the CDC given below).
Fourth, by now it is clear that there is no hard evidence to prove the effectiveness of lockdowns and several reasons to question it. The trigger for the lockdown measures was the Imperial College London (ICL) model of 16 March which predicted up to 510,000 UK and 2.2mn US deaths in “an unmitigated epidemic” (p. 7). The model described Covid-19 as “a virus with comparable lethality to H1N1 influenza in 1918” (the Spanish flu). Its assumption was that without intervention, 80% of the people would be infected and the IFR was 0.9%. In a subsequent interview lead author Neil Ferguson clarified that based on information “gathered in recent weeks… it has become increasingly clear that actually this is not the reasonable worst case, it is the most likely scenario.” The ICL model has been proven just as spectacularly wrong in its best-case scenario of a maximum of 20,000 UK deaths over two years with school and university closures, case isolation and social distancing, going down to 15,000 with home quarantine thrown into the mix as well (p. 14); the actual number of Covid-related deaths in the UK was already over 70,000 by the end of 2020. Similarly, responding to Nicholas Kristof of the NY Times (20 March), Ferguson predicted a best-case scenario of 1.1mn US deaths (against his model’s worst-case estimate of 2.2mn deaths).
There are strongly divergent views among software engineers, epidemiologists, medical scientists, physicists, chemists, and statisticians over the quality, reliability and predictive utility of the ICL model. Several medical-scientific-epidemiological experts questioned the mass hysteria and the panicky responses but were ignored, even though panic produces bad public policy. Sweden’s chief epidemiologist Anders Tegnell noted that shutting down and locking down have no “historical scientific basis.” John Ioannidis, one of the world’s most cited scientists, called the existing data on coronavirus infections “utterly unreliable” and dismissed much of the early epidemiological modelling as “speculation and science fiction” that had fed a “mob mentality.” In a meta-analysis published in the WHO Bulletin on 15 October, Ioannidis found the median overall IFR is 0.23%, but low and high mortality countries have IFR of 0.09% and 0.57%. For people under 75 it’s 0.05%. The global coronavirus IFR is thus broadly comparable to that of flu overall, significantly lower for most of the working age population, and close to insignificant for schoolchildren. School closures cause great harm for zero health gain for children or even the teachers. The BBC reported (28 August) on a large UK study that not one otherwise healthy under-19 child had died of Covid-19. The Guardian reported (20 October) worries from government scientific advisers that school closures would leave children “scarred for life.” The story is similar in the US, said the NY Times (22 October) and its columnist Nicholas Kristof (18 November).
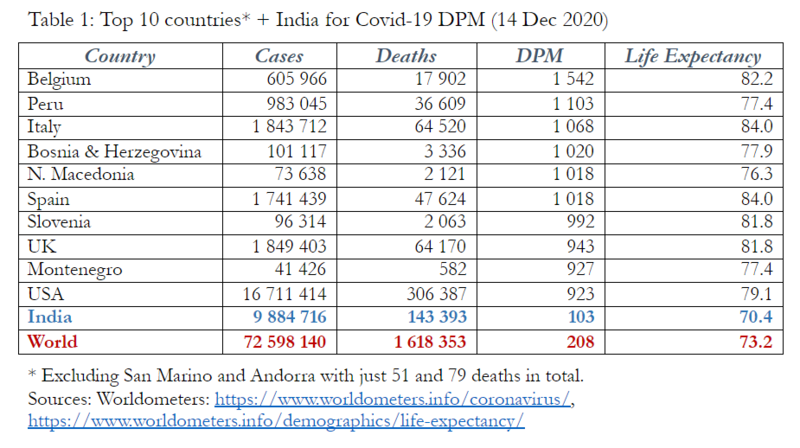
Yet, policy invariance has not reflected the highly age-segregated deadliness of the disease, despite the recommendations of the Great Barrington Declaration for “focussed protection” that had been signed by nearly 52,000 doctors and public health scientists and over 700,000 concerned citizens from around the world by year’s end. Every one of the top ten countries by Covid DPM (Table 1) has instituted lockdown measures. According to a study in EClinical Medicine published by Lancet: “Rapid border closures, full lockdowns, and wide-spread testing were not associated with Covid-19 mortality per million people.” However, “Increasing Covid-19 caseloads were associated with countries with higher obesity” and higher “median population age.” On US states, another study offered two conclusions: lockdowns didn’t help to contain the spread of the virus and opening up didn’t hurt. Confirming that, in late December a regression analysis calculated the coefficient of determination (R2) between NPIs and DPM to be 0.003 for the 50 US states plus DC, meaning that variance in NPIs has zero explanatory utility for explaining their variance in DPM.
The lack of covariance might provide an answer to this attention-grabbing headline from Politico on 23 December: “Locked-down California runs out of reasons for surprising surge.” Despite “some of the toughest restrictions,” California had become “one of the nation’s worst epicenters for the disease, setting new records for cases, hospitalizations and deaths.” This “has confounded leaders and health experts,” Victoria Colliver wrote. As Roger Koops says: ‘Stopping humans from being human will not stop the virus from being a virus!’ They should consider the possibility that the whole approach is flawed and the Great Barrington Declaration’s alternative approach, of shielding those most at risk while encouraging the rest to get on with their lives with sensible individual precautions, makes more sense. Meanwhile in San Francisco, 621 people died of overdose in 2020 compared to 173 with Covid-19.
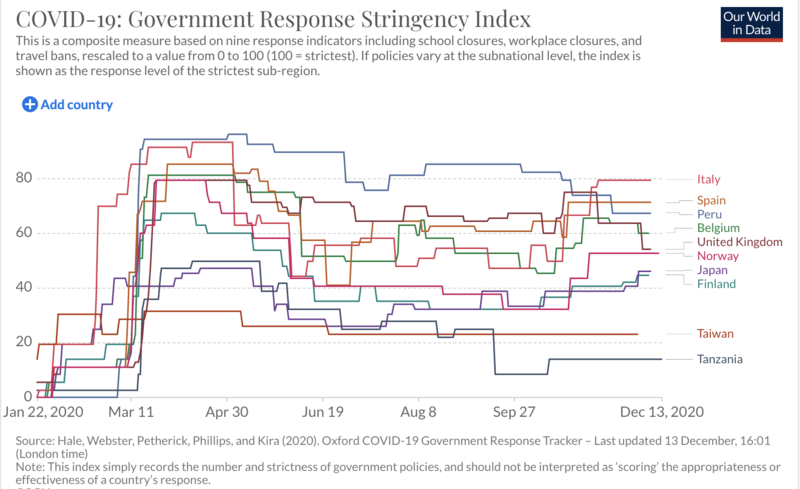
Forget causality; there’s not even a clear correlation in either direction. Countries that locked down hard and those that did not have widely varying mortality rates. Figure 2 maps the stringency index of ten selected countries. As the text below the chart notes, the five with the tougher lockdowns for prolonged periods have significantly higher DPM than the five with softer mitigation measures. In Europe and the Americas, outcomes invariance can be seen alongside a diverse array of policy responses. All this explains why Mark Woolhouse, professor of infectious disease epidemiology at the University of Edinburgh and a scientific adviser to PM Boris Johnson, said on 23 August: “Lockdown was a panic measure and I believe history will say trying to control Covid-19 through lockdown was a monumental mistake on a global scale, the cure was worse than the disease.” Bhopal warns that “striking fear into the minds of the people or punishing them… is not advocated in any public health strategy or international approaches to controlling the pandemic.”
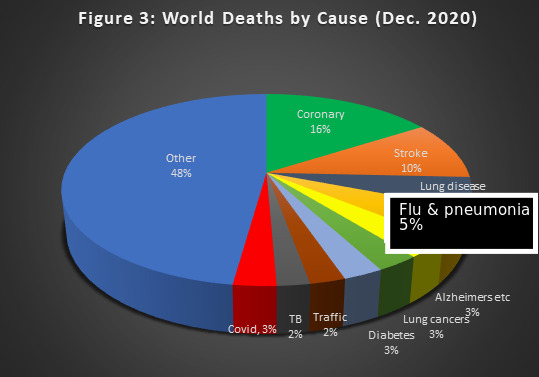
Fifth, it is abundantly clear that while coronavirus is indeed highly infectious, it’s not very lethal. The most common symptom is no symptoms at all, including 60% of new cases in China. As at 2 January 2021, the total number of cases in the world was over 84mn and 1.8mn people had died of Covid-related illness. Of 61.5mn closed cases, 3% had died. Of 22.8mn active cases, 99.5% were described as “mild” and only 0.5% as “serious or critical.” That is, it’s so vicious that millions must be tested to know if they’ve had it. The CDC figures for age-segregated IFR published on 10 September show that for those infected with coronavirus aged 0-19, the survival rate is 99.997%; 20-49, 99.98; 50-69, 99.5; and 70+, 94.6%. At around 80 years old, the average of Covid-related death is near and often above the national life expectancy. Not surprisingly then, Covid-19 accounted for less than 3% of all causes of global deaths in 2020, and even this is when including everyone who has died with the virus as having died from it (Figure 3). In other words, the lockdown interventions represent the biggest triumph of the Henny Pennys (or Chicken Littles) of the world in human history.
Sixth, the massive toll in other health outcomes, damaged economies, lost livelihoods, curtailment of human rights and civil liberties became clearer with each passing month. “Flattening the epidemic curve” came at the cost of flattening economies. A spate of reports from multiple intergovernmental, private sector and civil society sources warned of dramatic decelerations and contractions in GDP and trade from the pre-pandemic forecasts, with a resulting ballooning of poverty. In developing countries, the disruptions to national and global economic activities could reverse decades of progress for tens of millions on life expectancy, hunger alleviation, infant and maternal mortality, immunization and educational outcomes, child labour and sex trafficking, female emancipation from forced early marriages, and human dignity. Hence the conclusion from a Canadian medical practitioner: “If lockdowns were a prescription drug for Covid-19 treatment, the FDA would never have approved it.”
The 6-12% range for Covid-19 deaths without comorbidity (see above) means there never was any justification for turning a national health service into a national coronavirus-only service. Multiple reports documented the immediate and likely long-term economic harm caused by lockdowns; the risks of deferring consultations, screenings and surgery for other medical conditions; the impact of fear, enforced isolation, anger, frustration, financial loss and unemployment on mental health; and the added risk of domestic violence. Drs. Jay Bhattacharya (Stanford), Sunetra Gupta (Oxford), Carl Heneghan (Oxford) and Martin Kulldorff (Harvard) operate a useful website called Collateral Global as a global repository for research into the collateral effects of the Covid-19 lockdown measures on mental health, physical health, social health, education and the economy.
Seventh, in earlier epidemics (when scaled up to today’s global population, Asian Flu 1956–58 killed 3mn people; Hong Kong Flu 1968, 2.2mn; HIV/AIDS has killed upwards of 25mn since 1981), the numbers infected and killed were sufficient to produce a severe impact on society. But catastrophism on some previous epidemics proved false. In 1999, European scientists suggested up to 500,000 people could die from the UK mad cow disease. By October 2013, 177 deaths were recorded from the disease. In 2005, the UN’s coordinator David Nabarro warned between 5mn-150mn people could die from avian flu; WHO official estimates were 2mn–7.4mn. Only 455 people died of bird flu from 2003–2019. With the 2009 swine flu, instead of the feared 1.3% IFR, the actual rate was 0.02%, comparable to the US 2007–09 seasonal flus. In the UK, where the IFR was 0.026%, against the “reasonable worst-case scenario” of 65,000 deaths, there were only 457. The panicked government spent £1.2bn on flu remedies that were not needed. The WHO came under severe criticism for having served the interests of “Big Pharma” in selling unnecessary vaccines. The total worldwide deaths was about 280,000.
In all the previous deadly pandemic episodes, governments didn’t shut down their country, destroy the economy and jeopardize their way of life. People suffered but endured. This too shall pass. Walter Scheidel reminds us, in an essay in Foreign Affairs, that the ICL model’s hyperbole notwithstanding, SARS-CoV-2 is nowhere near as lethal as the Spanish flu that killed the fit and young as virulently as it did the elderly and infirm. It infected 500mn people (one-third the world’s population at the time) and killed around 50mn. Scaled up to the global population in 2020, that would translate to around 200mn-250mn dead today. The erosion of liberal democratic freedoms and sense of community and fellowship is another component of the trade-off equation. Human beings are family- and community-oriented social animals. Sharing food and drink at home or in restaurants, enjoying the cinema, watching football or cricket, appreciating a concert or a play are not optional add-ons but fundamental to our daily life as human beings. “Social distancing” by contrast is profoundly anti-social and rubs against every fibre of human civilization. From everything we now know, the elderly should be free to meet, greet and hug grandchildren under 10 to bring back joy and cheer to the lives of all three generations of a family. On 21 October, despite a modest rise in Covid cases, Sweden lifted all remaining restrictions on over-70s. The justification was not economic but emotional health. Health Minister Lena Hallengren explained: “We cannot only think about infection control, we also need to think about public health.” Months of social isolation had meant loneliness and misery and a “decline in mental health likely to worsen the longer the recommendations remain in place.”
Finally, Japan, South Korea and Taiwan have shown how democracies can manage epidemiological crises without rupturing society or sacrificing the economy: if you are sick, stay home if you can but if you must go out, wear masks in crowded settings and avoid physical touching and proximity; the East Asian bow and Indian ‘Namaste’ are simple, elegant, cordial yet respectful alternatives to the ubiquitous handshake; wash or sanitize hands frequently; check temperatures at airports, seaports and on entry into crowded areas like train stations, office complexes and malls; test those with elevated temperatures; hospitalize serious cases and quarantine those with symptoms at home with random inspections to ensure compliance; and trace and isolate those with whom they have been in contact.
The Pandemic in India
The survey of the global landscape on the spread and virulence of the coronavirus pandemic and the range of interventions by governments underscores the importance of striking a balance between health, social, and economic policies, as well as individual freedoms for citizens, in all their dimensions. The risk of creating mass hysteria and panic with exaggerated reporting must be set against the risk of losing control by delaying public announcements of the true scale, gravity and urgency of a nascent epidemiological emergency. A government must settle on the optimal balance between sufficiently slowing the disease, preventing an economic meltdown and maintaining a functioning society, while the threat and responses evolve and the virus spreads. It is our contention that in India, PM Narendra Modi went into a lockdown far too early and much too hard. It was imposed without adequate thinking about preparations relating to logistics and health infrastructure, and without any planning of implementation which could have been selective in geographical space and sequential in time. Such an approach caused unnecessarily brutal hardships that could have been softened with a more calibrated and targeted range of interventions.
As of 2 January 2021, India’s total number of coronavirus cases was over 10mn and deaths totalled 149,205. While this is the second and third highest in the world after the US and Brazil, in the context of India’s massive population and exceptionally high prevalence of many deadly illnesses, Covid-19 accounted for only 1.6% of the 9mn all-causes annual mortality in the country. Moreover, in line with global experience, 69% in India were asymptomatic in one survey conducted by the Indian Council of Medical Research.
However, India’s Covid-19 experience is anomalous in the global context for three reasons. First, its DPM is substantially below that of the Western countries and the world average (Table 1), but higher than both the Asian and South Asian averages. Although its mortality rate was only 103 DPM, the average DPM of its South Asian neighbours (Afghanistan, Bangladesh, Bhutan, Nepal, Pakistan, Sri Lanka) was just 41; and of East Asia (China, Hong Kong, Japan, Mongolia, South Korea, Taiwan) was under 5 (14 December 2020 figures). India’s real toll might even be higher. China is not the only country with question marks over the reliability of their Covid data. According to a BBC report, some of India’s states are undercounting Covid deaths, attributing them instead to comorbidities; others have weak health surveillance systems. There are reports of discrepancies between official tolls and counts from crematoria and burial grounds. The vast majority of Indians die at home, with last rites performed by the family. The fear generated by the alarmism around coronavirus has led to heavy stigmatization. Doctors and young Muslims have been refused burial for fear of being contagious. Families could be reluctant to take sick members for testing and hospitalization. Many who succumbed might be cremated or buried quietly, to avoid social stigma and ostracism.
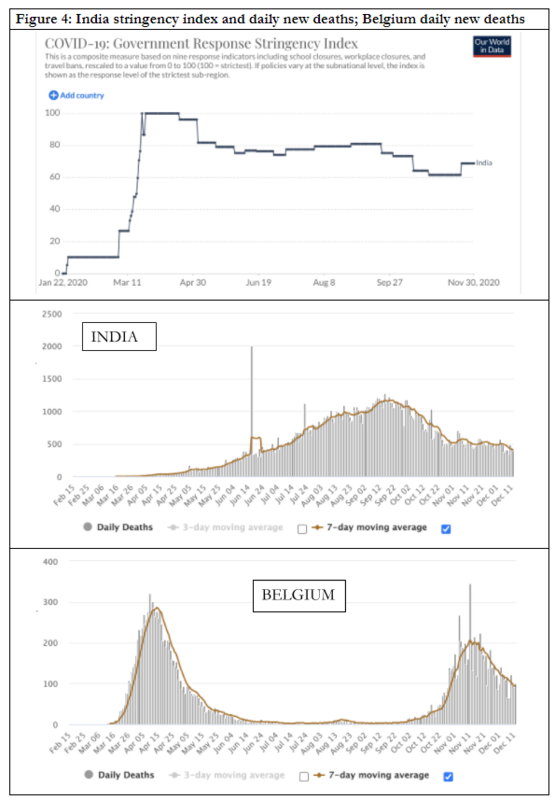
Second, in the typical seasonally fluctuating mortality curve of the worst-affected European countries like Belgium (Figure 4), deaths rose exponentially in the first month, then fell sharply although not quite as steeply over the next two months, remained flat through to the end of September and climbed steeply again in autumn. Nobel Laureate Michael Levitt postulated a “self-flattening curve.” Indo-British Oxford Professor of Theoretical Epidemiology Sunetra Gupta observed that rates of infection and mortality were strikingly similar across countries with different lockdown policies: they grew, stopped, turned around and retreated “almost like clockwork.” Europe and the US seem to offer more support for this thesis than for the original modelling that predicted indefinite exponential growth without stringent control measures. By contrast India’s curve shows an initially slow and then a steady rise through to the end of September followed by a slow descent, with little visible correlation with the stringency index line that began with 100 (maximum mitigation measures) on 25 March (Figure 4). There is little evidence of self-flattening.
And third, other countries locked down, watched their cases and deaths fall right down, and only then eased restrictions before re-imposing some measures again for the “second wave” in September. The discrepancy between the spike in infections amid a fatalities plateau seen across Europe and the US in autumn was striking, although Germany seems to be far worse in the autumn compared to the spring. The rise in infection numbers could be an artefact of increased testing, high false positive rates in testing, with ultra-sensitive testing possibly picking up fragments of dead virus from old infections. Or it might indicate improved treatment protocols and procedures, or even that perhaps population immunity has been achieved in some countries.
Although many now accept we may have to learn to live with the virus, epidemiologists, medical scientists and public health experts remain sharply divided over “herd immunity.” While the dominant assumption has been that the threshold for population immunity is 60-67% [based on the formula HIT(%)= (1-1/R0)x100, where HIT is the herd immunity threshold and R0 is the average number of other people that one infected person infects and is assumed to be 2.5-3.0], some now suggest in certain areas it could be just 20%–25%, possibly even lower. The complexities of real life showed clearly that some people are more infectious and more vulnerable to coronavirus than others, while an unknown but significant proportion are asymptomatic. As the highly susceptible and vulnerable get depleted in the initial wave, the spread of the virus decelerates. The spikes of the initial wave of infections are unlikely to be repeated in subsequent waves as the susceptible-vulnerable population has decreased. Also, even if our immunity weakens and fades and cannot prevent us from getting infected again, it may still reduce the severity of the disease, which itself could become less deadly in successive iterations. One study showed the infection rate in Mumbai slums was 57%, compared to 16% in other areas of the city. That is not surprising, because the slums lacked commensurate fatalities and physical distancing in crowded spaces was almost impossible. The fact that a substantially lower proportion of infected people were dying with Covid in the slums than elsewhere suggests that the threshold for achieving population (herd) immunity through infection might well have been significantly lower in the Mumbai slums.
India imposed total nationwide lockdown with a stringency index of 100 (Figure 3) on four hours’ notice on 25 March, without any advance logistical preparation to manage the consequences. The graphic emblems of India’s harsh lockdown included shuttered stores; deserted schools and universities; closed playgrounds and parks; beaches without people; empty markets; silent houses of worship; bankrupt businesses; and millions of migrant daily-wage labourers trekking home over hundreds of kilometres.
The harsh lockdown, at such short notice, created a humanitarian crisis of enormous proportions. The plight of migrant workers in urban India – construction workers, street vendors, restaurant employees, delivery persons, domestic workers, rickshaw drivers and so on – was grim. Deprived of their work and dignity, uncertain about where their next meal would come from, stranded in megacities, in search of night shelters and open kitchens run by state governments or charities, most of them were desperate to return to their home villages. But there were no buses or trains in the lockdown. Inter-state movements of people were prohibited. Yet, thousands of migrants set out on foot, carrying their children, to walk hundreds of miles, braving the sun, their hunger and the police. It was only two months later, when such a humanitarian crisis could no longer be ignored, that the government allowed special trains and buses to take the stranded migrants home.
The lockdown was meant to end on 14 April, but was extended three times until 3, 17 and 31 May. The unlocking process started hesitantly around 8 June. In substance, however, the near-complete lockdown continued until end-June, as several state governments continued the lockdown, while the embargos were lifted very slowly elsewhere. Some restrictions were lifted on 1 July but the lockdown continued to be stringent on the movement of people and in many other respects. Further relaxations and lifting of restrictions have continued to be announced on the 1st of each month since then. But schools, colleges, and other educational institutions remain closed. Cinemas, theatres, gyms, entertainment places and bars have been allowed to reopen but with restrictions to ensure physical distancing, so that business is far from normal. Public transport systems in cities have restarted but both frequency and use are far lower than before the pandemic. Passenger trains and domestic flights, too, are skeleton services compared with the past. International travel remains highly restricted to a few point-to-point bubble-flights. The economy that had almost shut down has begun to limp forward, but it will be quite some time before it can walk let alone run or hum with activity.
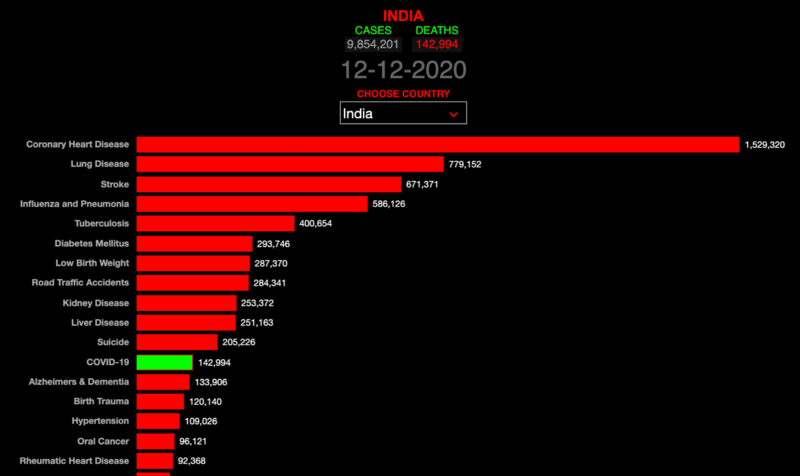
Yet among India’s biggest killers, Covid ranks 12th, well behind heart diseases, lung diseases, tuberculosis, diabetes, and traffic accidents (Figure 5). Of the 139,123 suicides in India in 2019, daily wage earners (25% of the workforce) numbered 32,563 (23.4%), rising steadily each year to double from 12% in 2014. The unemployed made up another 10.1%. With preliminary estimates of suicides already at over 200,000 by 12 December, we shudder to think what the final 2020 numbers will be. More importantly, it makes no sense to intervene to combat Covid with policy measures that increase the deaths from suicides that are already 43% higher than the coronavirus toll and at risk of almost doubling from 2019.
India has plummeted from the world’s fastest growing major economy to the fastest shrinking. Its GDP contracted by 23.9% for the April–June 2020 quarter, and by 7.5% in the July–September quarter. Even if the next two quarters are better, projections suggest that GDP will contract by about 10% in 2020–21: among the sharpest contractions in the world.
The harsh lockdown smashed the economy. Yet, migrant labourers, driven out of many cities, spread the disease deep into India’s village heartland when they returned home. India got the worst of both worlds and is yet to recover on either the disease or the economy front. Its housing, water and sanitation realities are a nightmare for any epidemic that is both highly infectious and lethal. Physical distancing is impossible in slums where generations of families sleep in one room, eat together and share communal water and sanitation facilities. The situation in villages differs only slightly on the physical spread of housing.
The biggest killer in today’s world is not any one disease or a pandemic, but poverty. The health of most people is vitally dependent on a healthy economy that gives the government the financial muscle to create an efficient universal-access public health infrastructure. The world’s bottom billion subsist in a Hobbesian state of nature where life is “nasty, brutish and short.” The human and economic costs of coronavirus will be far more devastating with low state capacity, weak health systems, teeming slums, multigenerational housing, unclean water and sanitation systems, congested mass transit, and inadequate safety nets. The killer ailments that are taking the heaviest toll are water-borne infectious diseases, nutritional deficiencies and neonatal and maternal complications. Few Westerners realize that the biggest death toll even from the 1918 pandemic – between one-fourth to one-third of the world total – was in India.
The Indian government’s relief packages were too little and too late. For example, the package announced on 12 May was insufficient to alleviate the distress in the agricultural, airlines, automobiles, hotels, restaurants and tourism sectors. Nor was it much help to the poor and migrants in shielding them from the harsh realities of hunger without jobs, incomes, shelter or dignity. The economy was flattened by the contraction of output on the supply side and contraction of employment on the demand side. But government measures have focussed on the supply side while neglecting the demand side. This showed a flawed understanding of economies in crisis and little recognition of the reality when a prolonged lockdown has brought the economy to the edge of collapse. Without expansionary macroeconomic policies, there is a serious risk that the economy will go into a free-fall. In that case, the shortfalls in public revenues would cause the fiscal deficit to balloon without any hope of recovery. Survival through the crisis was essential for the return both of poor households and small firms to economic activities. The short-term stabilization focus should have been on households on the demand side and firms on the supply side. In the absence of such correctives, recovery, whenever it begins, is most likely to be K-shaped, in which things get better only for a small proportion of the population (comfort for the rich) but remain unchanged or get worse for most people (hardship for the poor).
Thus, the lockdown has produced its own socioeconomic version of Thucydides’ geopolitical dictum that the strong do what they can, the weak suffer as they must. The virus carriers were the wealthy, but the poor bore the burden. The privileged jet-setters who imported the virus could work remotely from home and utilize the private hospitals. But the poor they infected, who depend on daily wages from manual labour and have little access to decent healthcare, were disproportionately devastated. The lockdown shuttered almost two-thirds of the economy. It stranded 25-30mn migrants in cities far away from their homes, deprived of their work and dignity, at the mercy of food and shelter provided by state governments or charities, often hungry and homeless, creating an unprecedented humanitarian crisis. Manufacturing, mining, construction, trade, hotels and restaurants, and transport, which account for more than 40% of both output and employment, were shut down completely. Thus, 150mn people, as much as one-third of the total workforce, who are casual labour on daily wages or workers in informal employment without any social protection, were deprived of their livelihoods. Much of this burden was borne by the poor, often self-employed, who constitute 75% and 50% of rural and urban households respectively. The impact on micro, small and medium enterprises, which account for 32% of output and 24% of employment in India, was devastating. Healthcare for patients, except for those with Covid-19, diminished sharply in terms of both access and quality. In education, learning outcomes, which are already poor, are bound to get worse with school and university closures.
Like most strongmen, Modi has prioritized the expansion and consolidation of state power over the development of state capacity. India’s economic slowdown began long before the pandemic hit and there was little to cushion it from the lockdown’s harsh impact. The neglect of urgently needed economic and governance reforms in order to pursue a religious agenda left the country exposed to the exogenous shock. Democratic India used brutal tactics to enforce one of the world’s harshest lockdowns, for example by spraying desperate migrant workers with chemical disinfectant.
On the one hand, the high level of trust that the Indian public has in Modi, premised on the belief that he acts in the national interest instead of for personal or family profit, gives him room for tough and decisive action. On the other hand, weak capacity in turn means that authorities will have correspondingly greater difficulty in case management and contact-tracing. India has the world’s biggest pool of poor, illiterate, sick, hungry, underweight and stunted children, as well as of sexual assault and domestic violence victims. Widespread poverty diminishes the state’s capacity to provide adequate nutrition needs of its people and being malnourished makes people more vulnerable to coronavirus. The equation has clear if uncomfortable implications for all countries with poor public health infrastructure. The government has a critical and indispensable role to play in public health during pandemics: prompt, accessible and affordable universal testing, ramped up hospitals to cope with a surge in demand, accelerated supplies of protective, preventive and therapeutic medicines and equipment, etc. Poverty hollows out state capacity to do all this.
The long-term impacts of the lockdowns will be deadly for the world’s poorest billion people over the next decade. Oxfam warns the pandemic could push another half billion people into poverty. The number of people suffering from acute hunger could nearly double to 250mn from the disruptions to crop production and global food distribution chains. Grave and prolonged economic damage takes its own tragic toll on lost livelihoods and on lives. This is seen at its most acute and more immediately in developing countries whose people “fear hunger may kill us before coronavirus.” The United Nations estimates the global economic downturn could cause “hundreds of thousands of additional child deaths in 2020.” Other UN estimates show that more than 800,000 Indian infants died in 2019, a mortality rate of 3%. Nearly 1mn children under the age of 5 years died, an even higher mortality rate of 3.7%. Those figures are ten times higher than the infant and child mortality rates in the developed world. Most of these Indian children died from preventable causes – nutritional deficiencies, lack of sanitation and lack of access to healthcare.
Exit from a lockdown poses a tough dilemma for governments. It requires decision-making under high uncertainty and courage grounded in both conviction and confidence. The belief of orthodox economists in the strong spring analogy – the harder you push an economy down, the greater the force with which it bounces back – is an illusion. In reality, a weak spring is the more appropriate analogy for a poor economy. If pushed too hard, it may simply remain down if its restorative forces have been destroyed.
The impact of diseases can and does differ across countries and continents, possibly attributable to differences in demographics, geographies, cultures and immunities. A study covering 290 hospitals in all 30 districts of the state of Karnataka in India was preprinted online on 11 December. Billed as “the first comprehensive survey providing accurate estimates of the Covid-19 burden anywhere in the world,” its estimated IFR was just 0.05%. India has a much younger population than rich countries, so that the proportion of vulnerable people older than 65 years is far lower. Countries like India which have mandatory BCG vaccinations may be less susceptible to Covid-19 infection because the vaccine has a stimulating effect on the immune system that goes well beyond tuberculosis. In India, universal BCG and polio vaccination is mandatory, while immune systems of people have a lifelong exposure to curative and preventive drugs for malaria. The conventional assumption is that vaccines create antibodies against specific pathogens. But immunologists have discovered that vaccines also stimulate innate immune systems creating capacities to better resist, or fight, other kinds of pathogens too. This possibly exists in immune systems of people in India who have antibodies that could be effective in resisting the virus. Similarly, the significant number of people who have tested positive for Covid-19 but are asymptomatic suggests that they have some innate T-cell mediated immunity which helps resists the virus. Research by Indian scientists suggests that exposure since childhood to an extensive range of pathogens has given Indians relatively sturdier immunity to Covid-19. Another study in the International Journal of Infectious Diseases suggested a similar conclusion holds for sub-Saharan Africa.
Lockdowns, combined with mass testing, contact tracing, containment zones and mandatory quarantines, can only slow down the speed at which the infection spreads. This might help for temporary periods in countries where public health facilities are robust, but is inadequate for large numbers when infections peak. India’s public health system is poor and it could never suffice for its large population if the pandemic spreads. It could still be some time before vaccines become available in sufficient quantities to suffice for India’s massive population. On 2 January 2021, the expert committee of the Drug Controller General of India recommended restricted emergency authorization for the Oxford-AstraZeneca Covishield and India’s indigenously-developed Bharat Biotech’s Covaxin vaccines. Because “the initial vaccine supply … is likely to be very slow,” however, “for the average Indian aged less than 50 years and without any comorbidities, the wait for a jab is likely to extend till 2022.”
It is also essential to recognize that a lockdown is not a weapon in a war that can conquer or vanquish the microbe. The virus will be with us for some time to come and there could be a spike in infections when the lockdown is eased, and such spikes may recur over time and across space. India must learn to live with this reality of an endemic equilibrium, just as it did with pneumonia, and manage the virus as best it can. There is also the possibility that yet another novel virus could emerge, potentially reigniting a perpetual process of unfounded fear and revolving-door lockdowns. Last but not least, this is a wake-up call to improve social infrastructure on public health, which would save lives lost through easily preventable causes, for example child mortality, to bring about significant improvements in the wellbeing of the people.
India’s potential global role
Like any crisis, the pandemic presents its own opportunities. India has the potential to play a more prominent role in the rapidly shifting and fluid global order as a low-cost manufacturing hub of safe, reliable and inexpensive but essential medicines. As countries prepare to end overdependence on China for critical medical supplies, the post-Corona world will offer India, already a leading global actor in the pharmaceutical industry, an unexpected, longer-horizon opportunity to play a larger role in revamped global supply chains, expand its manufacturing base and become the pharmacy to the world. The deindustrialization that India has witnessed over the past quarter century, because of unilateral trade liberalization while abandoning industrial policy, could be reversed. The rhetoric of “Make in India” could be turned into reality, if India began manufacturing for world markets as large international firms relocate production out of China.
This would require the government to formulate strategic industrial policy that coordinates trade, technology, fiscal, monetary and exchange rate policies for reviving industrialization. It would also require massive investments in physical infrastructure, particularly power, roads, transport and ports. This should be done without moaning about finances, for it would serve two purposes. Government expenditure on infrastructure creates employment and stimulates demand to revive economic growth in the short run and removes supply constraints that would stimulate the economy through strong multiplier effects in the long term.
For example, India is the largest producer of hydroxychloroquine as the drug is commonly used to treat malaria which is widespread in India, manufacturing 70% of the world’s supply. India is also the world’s largest producer of vaccines and has enormous experience in implementation of mass vaccination programs for smallpox, BCG, polio, etc. On 19 April Modi exhorted India to rise to the occasion and become “the global nerve centre of … multinational supply chains in the post Covid-19 world.” In his virtual address on 26 September to the UN General Assembly’s 2020 opening session, Modi proudly noted that India’s pharmaceutical industry had sent essential medicines to more than 150 countries. He then promised: “As the largest vaccine-producing country of the world, I want to give one more assurance to the global community today, India’s vaccine production and delivery capacity will be used to help all humanity in fighting this crisis.” With the right industrial policy, some Indian pharmaceutical companies, which already have an established presence in the world market and compete with subsidiaries of US and European firms in the domestic market, could become global firms.
India could also take a lead in resisting the climate of pandemic nationalism unleashed by the “My Nation First” mentality. When the Brundtland Commission Report (1987) said “The Earth is one but the world is not,” hardcore realists dismissed that as the romantic notion of dreamers. Yet the serial crises of the last few decades, from natural disasters to pandemics, from financial meltdowns to terrorism, remind us that no nation can be an island, sufficient unto itself in the modern world. The pandemic and lockdowns together posed an unprecedented threat both to public health and to the global economy. US President Donald Trump’s disruption of the global trading order made it correspondingly more difficult to organize a coordinated response to the pandemic or for the US to provide the requisite world leadership. The rushed retreat into “beggar-my-neighbour” responses, where Washington tried to buy exclusive access to vaccines produced in Germany, forcefully demonstrated the consequences of the crumbling architecture of the global order. ‘Sicken-thy-neighbour’ policies led dozens of countries to impose restrictions, including outright bans in some cases, on the export of critical medical supplies like masks, medicines, ventilators and disinfectants. Espousing nationalist rhetoric and policies, while abandoning international cooperation, aggravated the crisis. Governments can better protect the people they claim to represent by reversing the equation – ditching pandemic nationalism and embracing global cooperation instead.
Thus, the pandemic reaffirms the importance of looking for solutions without passports to problems without passports. The media was flooded with predictions that the pandemic will kill globalism. The death of globalization and global institutions is much exaggerated. A universal pulling up of drawbridges behind national moats would do collective self-harm. The positing of national sovereignty and UN-centric multilateralism as alternatives is a false dichotomy. We need both strong state capacity, not power, at the national level and efficient and effective multilateralism for coordinating responses at the global level. The ethic of collaboration can be operationalized through the UN-centred mandated multilateral machinery such as the WHO, voluntary international organizations like the Non-Aligned Movement, BRICS and the G20, regional intergovernmental organizations, philanthropic foundations and private sector initiatives. India’s potential as the pharmaceutical manufacturing hub gives it the parallel scope to provide global leadership in organizing collaborative efforts that can be institutionalized instead of depending on ad hoc responses with each fresh crisis.
In sum, the crisis is a sharp reminder of the limits of unilateralism and cascading vulnerability to external shocks in an age of shared threats and fragility but unequal resilience. National adequacy measures must be supplemented with building international functional redundancy in food supplies, health and value chains in a deliberate strategy of “risk reduction through diversification.” It is in all countries’ individual self-interest to recreate a healthy rules-based international order that breaks down barriers to the free flow of masks, protective gear, test kits and other medical supplies.
Covid-19 has demonstrated the urgent imperative to reboot the ethic of global cooperation. Tackling a pandemic requires cross-border good governance: robust surveillance to detect, test, isolate and treat every serious case; unimpeded flow of medical equipment and supplies from manufacturing origins to affected countries; real-time intelligence sharing and exchange of best practices; and an impartial, technically competent and publicly credible international organization to establish universal health norms. An efficient and legitimate architecture of global health governance would have detected the emerging epidemiological threat early, sounded the alarm and coordinated the delivery of essential equipment and medicines from point of manufacture to population clusters in most need. There is a need for an early-warning system to detect the emergence of new or mutated viruses. An early Covid-19 warning enables a government to react rapidly by ramping up testing and engaging the whole population in contact tracing and containment, thereby potentially reducing the economic and social costs of an outbreak.
The faster and more effectively that we act to contain the spread of the virus in the world’s poorest and most populous countries, the better we can protect everyone. Unless large countries such as China, India and Indonesia are all coronavirus-free, the risk of re-infection will persist even in the global North and it will pose an epidemiological and economic threat everywhere, as the letter from Gordon Brown, Kevin Rudd and a large number of other leaders and prominent public figures warned. This requires urgent investments in prevention that also depend on international cooperation – including via the Africa, EU and US centres for disease control and prevention, the International Monetary Fund’s emergency financing and the World Bank’s emergency health support.