Abstract: Japan has one of the highest rates of hepatitis C virus infection in the industrialized world. This endemic and the challenges it poses for the future of Japan’s healthcare system stem, ironically, from the formation of a modernist settlement beginning in the late 19th century. Modern techno-scientific solutions to political problems inadvertently provided millions of opportunities for hepatitis C to spread in rural communities, among leprosy communities, the traumatized postwar community and into the national blood supply.
Late on the morning of March 24, 1964, Edwin Reischauer, President Kennedy’s ambassador to Japan, stepped through the front door of the U.S. Chancery building in Tokyo and headed towards a waiting Cadillac that would take him to a meeting with Kim Jong-pil, a South Korean politician and founder of the South Korean Central Intelligence Agency. Suddenly, a young Japanese man wearing a raincoat and thick-lensed spectacles darted up and stabbed Reischauer in the right thigh with a 6-inch kitchen knife. The wound was deep and bled profusely: Reischauer’s femoral artery had been severed. Embassy officer, John Ferchak, used his necktie to make a tourniquet, probably saving the ambassador’s life. Four aides quickly bundled Reischauer into the limousine and the car took off for the nearby Toranomon Hospital. There, Japanese surgeons worked for four hours to repair the damage to Reischauer’s leg. In the course of the surgery, he received several blood transfusions.
 |
The next day, Reischauer released a statement to the press in which he said in part: “I was born and grew up in Japan, and now that I have received Japanese blood, I finally feel I have become half Japanese.”1 But the transfusions had not only made Reischauer half Japanese, they had also infected him with the hepatitis C virus (HCV). He had been given what the Japanese were calling “yellow blood.” Three weeks later, recovering at Tripler Hospital in Honolulu, he displayed all the symptoms of acute hepatitis. In retrospect, this was almost certainly the acute phase of HCV infection, but since the hepatitis C virus was still far beyond the limits of scientific knowledge and the incubation period for hepatitis was not supposed to be so long, U.S. Army doctors diagnosed mononucleosis. Twenty-six years later, becoming half Japanese caught up with the founding father of postwar Japanese studies: after many years of debilitating illness caused by chronic HCV infection, Reischauer died of HCV-related cirrhosis and hepatocellular liver cancer. In the end, becoming more Japanese killed him.
In 1964, HCV infection via direct blood-to-blood contact with contaminated blood was happening wherever medicine could afford transfusion technology and wherever blood products and hypodermic syringes were in use as therapies or therapy delivery systems. Although the hepatitis C virus probably originated in West Africa in the late 15th century, its global sweep and pandemic status in the world today are both intimately linked with progression of the modernist settlement: the dualistic epistemological structure of modernity in which science and technology are divided from and purified of culture and politics. In the late 19th and early 2th centuries, this Platonic, post-Enlightenment settlement produced public health programs in North America and in Europe that were then exported into colonized territories as pure science without reference to their engagement with the political practice of imperial hegemony. If the results of unwitting introduction of European infectious diseases into 17th, 18th and early 19th century America and Australia were genocidal for indigenous populations and cultures, the depoliticized delivery of public health vaccination, fertility management and disease eradication programs in colonized or subaltern communities between 1918 and 1989 was a modernist vehicle for both demographic and disease outcomes that would not become apparent until decades later.
Perhaps this latter consequence of a modernist settlement is nowhere more apparent than in the political epidemiology of hepatitis C virus in Japan, where the political problem posed by the possibility of domination by the Euro-American powers between 1854 and 1945 was countered by resort to intense techno-scientific solutions increasingly set apart from social and cultural matters as time went by. Amongst these solutions were a nationwide public health project, a pharmaceutical research and marketing project and adoption of medical technologies for delivery of public health services and pharmaceutical products. From these solutions came Japan’s 21st century hepatitis C endemic. Among wealthy industrialized states, Japan has one of the highest rates of chronic hepatitis C virus infection: about 2.3 percent of the population bear the virus whereas in the United States, HCV infects about 1.8 percent; in nations such as Germany and Australia, 1 percent or less live with chronic hepatitis C infection. Japanese are four times more likely than Americans to develop liver cancer,2 and more than three quarters of all cases of primary liver cancer in Japan are caused by chronic hepatitis C virus infection.3 Since liver cancer is very difficult to treat, the great majority of people diagnosed do not survive without liver transplantation. Hepatitis C infection also produces a host of other disabling syndromes and conditions: cirrhosis; acute fatigue; lymphoma; depression; cognitive deficit; blood and skin disorders. The economic, personal and social burdens of chronic hepatitis C virus infection are thus very heavy.
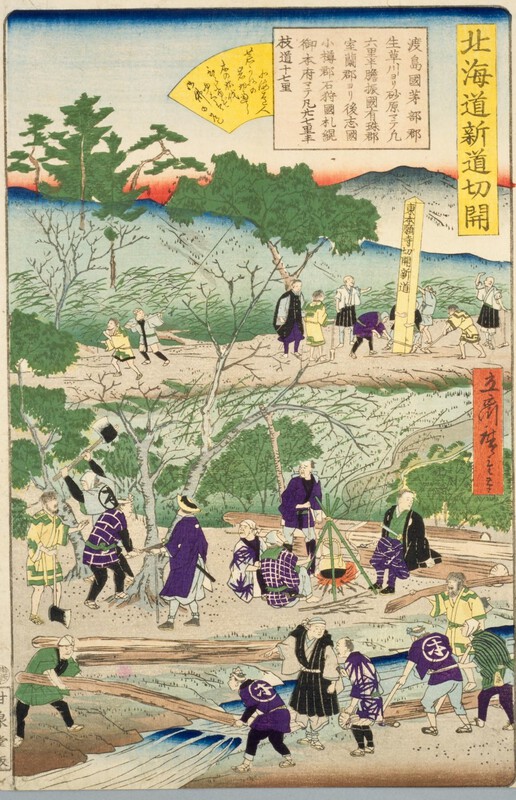
Working back from the current endemic, we can track a political epidemiology of HCV infection in Japan that comes directly from the local modernist settlement. In the period from the arrival of Perry at Edo to the surrender in 1945, Japan’s modernizers were remarkable for all the qualities noted in modernists by the historian of science, Bruno Latour: daring; research; innovation; tinkering; youthful excess; increasing scale of action; acceleration; multiplication of modernizers; creation of stabilized objects independent of society.4 And yet there were sometimes catastrophic consequences from modernist techno-scientific solutions to the problem of how to keep Japan out of the clutches of the West and elevate it to the status of modern world power. One of the most admirable of these modernists was Sensai Nagayo, but his solutions also led to the spread of hepatitis C virus in Japan. In 1871, Sensai was an eminent physician practicing in Nagasaki, but he was called to Tokyo and asked to join the Iwakura Mission, a group of scientists, and policymakers charged with scouring the world for technologies, practices and ideas that might be brought back to Japan and used to construct a modernist settlement.
Sensai Nagayo, the father of public health in Japan. |
In Germany, Sensai encountered the science of public health expressed in the complex German concept of Gesundheitpflege or “Hygiene” which at the time was also quite new to European modernists. “I heard ‘sanitary’ and ‘health’ everywhere and, in Berlin, ‘Gesundheitsphlege.’” Sensai later wrote. “But I did not really understand these words. Eventually I came to understand that these words meant not only protection of the citizens’ health, but referred to the entire administrative system that was being organized to protect the citizens’ health — a system that relied not only on medicine but on physics, meteorology, and statistics, a system which operated through the state administration to eliminate threats to life and to improve the nation’s welfare.”5
Much enthused by his discoveries and charged with modernizing Japan, Sensai took Gesundheitpflege and the rest of the package back to Tokyo with him. Initially, the new public health solution was directed at control of epidemic infectious diseases, such as cholera. In 1875, the government appointed Sensai head of Eiseika, a new Central Sanitary Bureau within the Interior Ministry. From there, he turned the imported Gesundheitpflege complex into a series of Japanese techno-scientific solutions dedicated to making the young nation state richer and stronger. In 1877, he issued scientific guidelines for prevention of cholera and began to promote national vaccination programs. Local Eiseika were set up and Sensai populated each Japanese ken and fu administrative district with an eisei-iin or Sanitary Officer. Sensai also played a leading role in production of a Japanese pharmacopoeia, thereby putting control of the science of drug compounding in the domain of government and, by regulating imports of drugs, promoted the science and technology of drug design and production in Japan: Japan’s pharmaceutical industry began here in this particular modernist solution.6 By 1895, the Eiseika had also mastered the science of statistics, presenting the health of Japan in sophisticated sets of graphs and tables.
Even so, the modernist settlement was not readily accommodated in Meiji Japan, thanks to anxiety associated with the idea that while science was intrinsically Western, Japan’s goal was to be free of Western hegemony. But, victories over China in 1895 and over Russia in 1905, colonization of Taiwan and Korea, along with a sustained explosion of heavy industrial development and associated techno-scientific massification during World War I, quelled this anxiety and made possible a modernist settlement involving the separation of pure universal sciences and technologies from culture and society in Japan. It was during this time too that the public health system and its technologies were turned on schistosomiasis (also known as bilharzia), inadvertently triggering the spread of the hepatitis C virus. Schistosomiasis is a disease once endemic to several local areas in Honshū and Kyūshū. It is caused when the schistosome trematode, a fluke worm which breeds in water snails, enters the human body and lays eggs there, causing a range of serious and sometimes fatal diseases affecting the liver, the gut and/or the renal and genital organs. Among diseases caused by parasites, schistosomiasis is second only to malaria in terms of the number of people it makes ill, and it is still endemic in parts of Africa and Asia. In Japan, Fujii Yoshinao, a physician practicing in wet rice rural areas of Hiroshima, described schistosomiasis in 1847 and gave it the name “Katayama disease.” By the end of the 19th century, public health authorities knew that schistosomiasis was endemic in the areas of Hiroshima Prefecture adjacent to the Takaya river, along the tributaries of the Fuji river in Yamanashi between Tokyo and Shizuoka, and around the Chikugo river in the Saga/Fukuoka region of Kyūshū. Hundreds of thousands, perhaps millions of Japanese sickened and died from the disease.
By 1978, however, schistosomiasis had been completely eradicated in Japan. Its banishment was a great victory of the modernist settlement in Japan, but it also broke down centuries of barriers to spread of the HCV virus. In the roughly four hundred years since the ancestor hepatitis C virus emerged in 1476 in what is now the West African republic of Guinea-Bissau, HCV had been relatively confined in the world by its requirement for direct blood-to-blood contact for transmission. Although it is likely that gory battlefields and the bloody, dirty ministrations of military surgeons provided opportunities for spread of HCV, and some sort of hepatitis epidemic was widely reported during Napoleon’s campaigns in Egypt and during the American Civil War, the spreads were highly localized and well contained; the means for endemic spread were simply not available. So too, in Japan, where the virus probably entered between 1880-1889, perhaps from an American ship,7 but at first lacked the means for great horizontal transmission. The resolution of the modernist settlement in public health science and technologies, however, dismantled barriers to HCV endemicity. By 1918, modern drug delivery technologies, such as hypodermic syringes and intravenous injections, which multiplied the number of opportunities for blood-to-blood contact, were in ever widening use in Japanese hospitals, in doctors’ offices and even in homes.
These modern tools in modern infection control programs were used on a massive scale to tackle schistosomiasis in Japan, thereby opening up millions of opportunities for the virus to spread horizontally. In 1917, John Christophersen, a British physician working in British Sudan, had discovered that repeated intravenous injections of antimony sodium tartrate killed the eggs of the schistosome in infected patients. Within a few years, British public health authorities had put in place a vast program of repeated intravenous antimony sodium tartrate injections throughout both Egypt and the Sudan. Starting in 1923, public health authorities in Japan followed suit. Using antimony sodium tartrate at first, and then a locally developed drug called Stibnal, the Eiseika (Sanitary Bureau) and health officials attacked schistosomiasis with such thoroughness that by the 1970s, public health officials had given more than 10 million intravenous injections to treat the disease in Japan.8 The schistosomiasis eradication project was a testament to Japan’s modernity, but something went invisibly wrong: public heath workers delivering schistosomiasis intravenous injections used and reused glass and steel syringes and needles. These were either not sterilized after each use or, if they were sterilized, were not sterilized in a way that destroyed the hepatitis C virus. Witlessly then, the modernist techno-scientific solution for schistosomiasis relentlessly spread HCV. By the 1930s, hepatitis C virus saturated communities where schistosomiasis once flourished. And from these localized zones of endemicity, the bolus of infections spread out from Saga, Hiroshima and Yamanashi, into adjacent communities.
Perhaps hardest hit by this spread of HCV was the incarcerated community of “lepers”9 in Japan. By the time HCV found it, the Japanese leprosy community was already much transformed by science and technology, and although these transformations have been discussed and examined at length in both Japanese language literature and in western accounts, to understand how hepatitis C and leprosy were brought together by the modernist settlement in Japan, it is necessary to recapitulate what happened with leprosy which until the 1980s, was mienai byō in Japan: the disease that cannot be seen. This problem of vision leprosy shared with chronic HCV infection, except that HCV infection is both asymptomatic until the end and could not be seen by science until after 1989, while leprosy can be so painfully visible that it has historically been hidden away. If any society could find a way of thinking that makes a noseless face beautiful, it is Japan where nodes of culture are organized around appreciation of the beautiful and around making the sad and the ugly seem lovely.10 But the horrible visibility of leprosy was recalcitrant, unredeemable in its ugliness. It had to be concealed, eyes had to be averted. Thus, from the time of leprosy’s first recorded appearance in 8th century Japan, governments sought to strictly regulate it. “Lepers” were usually obliged to live outside the village, the castle town and the great city: the disease was often viewed as a kind of punishment for sin, unskillful conduct and its karmic consequences. Nonetheless, before the 1850s, “lepers” were also a part of the overall community and autonomous leprosy communities were a common feature of life in Tokugawa Japan. Members of these communities exploited their status as karmic sinners to maintain autonomy and to survive. As Susan Burns writes: “They supported themselves by soliciting alms house-to-house several times a year: as they moved from home to home collecting offerings of rice, goods and cash, the ‘lepers’ announced themselves with the call ‘monoyoshi’, signifying that they were bringing fortune to those who showed them compassion.”11
This careful mix of seen and unseen, sin and forgiveness characterizing much of leprosy life fell apart quickly and in parallel with the falling apart of the Tokugawa state upon the unregulated arrival of mid-19th century modernity on Japanese shores. As bakufu power broke down after the shogun succumbed to demands for treaties and trade with the United States and the European powers, so did the power to discipline the visibility of leprosy and the movements of Japan’s 500,000 to 1.5 million “lepers” decline. Support systems for leprosy communities also stopped functioning. “Lepers” hit the road seeking alms and food, and with the whole land in a great and fracturing confusion, the shogun’s many and rigorously policed internal barriers to travel through the Japanese archipelago could no longer inhibit “leper” movement.
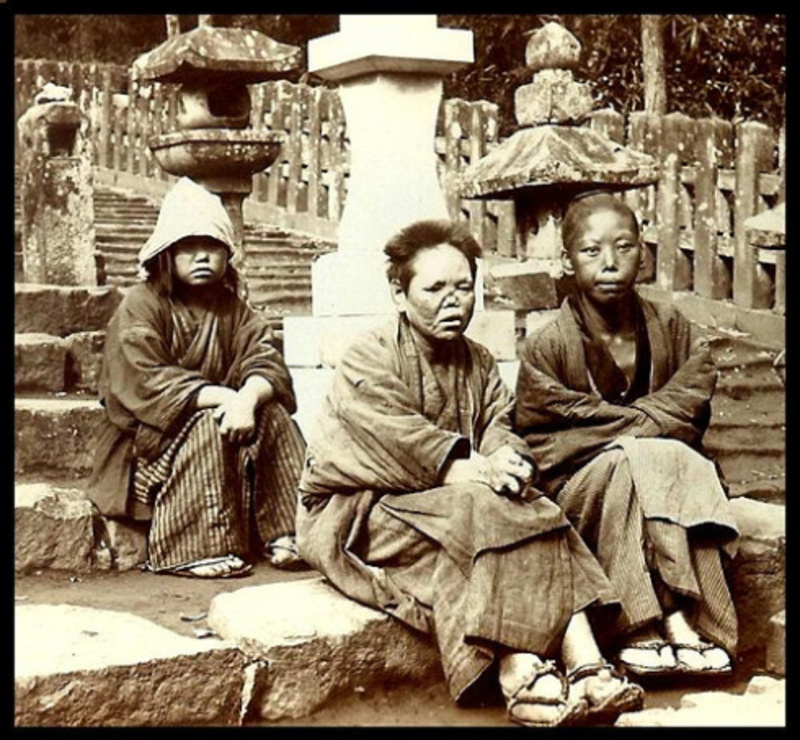
The horrible visibility of leprosy in Japan: Date and source unknown. Found here. |
Leprosy now appeared unregulated and “lepers” appeared in great conglomerated numbers in cities. People with leprosy walked the streets willy-nilly. They gathered at temples and shrines to beg for alms, displaying “the horrific morbidity of leprosy for the first time: the severely disfigured faces and nodulated bodies, the ceaseless groaning of a man with painful neuralgia, and the labored breathing”12 of those whose throat and bronchi were filled with leprous nodes.
Opening to the modern world tore up the existing contract between Japanese “lepers” and the state, setting “lepers” free, making them visible. Yet, as modernity began to settle on the land the unregulated display and movement of leprosy could not be allowed to stand. The problem was fundamentally political: “lepers” on the streets were a sign of Japan’s lack of modernity and until that lack was resolved, unequal treaties and vulnerability to Western hegemony could not be overcome. The solutions were techno-scientific and when they were delivered, they seemed almost completely divorced from and purified of the political problem. By the end of the 19th century leprosy was in abeyance in Europe and North America and when it was not, it was strictly and scientifically secluded. In Europe, Australia, and the United States, incarceration corrected the problem of visibility, provided a scientific solution to the threat of contagion and made administration of medical and behavioral technology to the body of the “leper” more manageable. Now these solutions were to be part of the modernist settlement in Japan and they were to be spearheaded by expatriates who believed that the scientific way to deal with “lepers” was to hide them.
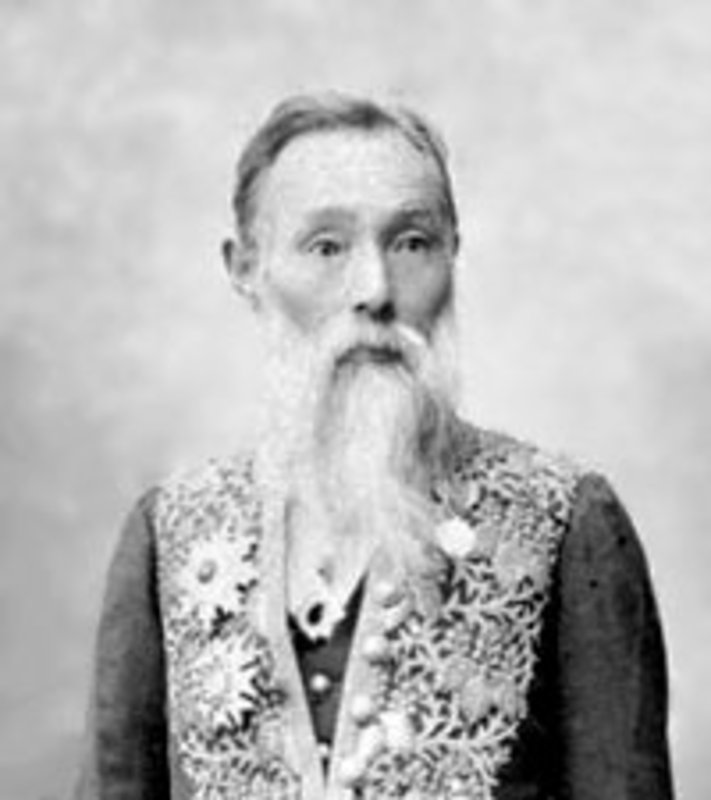
Foremost among expatriates pushing for removal of lepers from sight in Japan was a tall English spinster: Hannah Riddell. Imperious, independent and fond of luxury, Riddell came to Japan as a missionary when she was 35 years old.
Her posting was to the city of Kumamoto in Kyushu, and it was at Kumamoto in 1891 that Hannah Riddell first saw leprosy and was quickly struck with a complex urge to modernize Japan by removing “lepers” from sight, incarcerating and regulating their every movement and moment. Her encounter came during a visit to the splendid Nichiren sect temple of Honmyō-ji north of the city. At the top of the two hundred steps leading up to the main temple hall and the tomb of Katō Kiyomasa, 16th century lord of Higo and hero of the 1592 to 1598 Japanese attempt to conquer Korea, Riddell came upon leprosy and its bearers. In her retrospective accounts of this initial sighting, it is all about the visibility of leprosy and the stain the lepers at Honmyō-ji made upon beauty: “It was in the spring about ten years ago that I came to this temple for the first time. That day happened to be one of its annual great festivals. The sky was clear and bright and the cherry blossoms were at their best for quite a distance on either side of the road. Under the beautiful blue sky and the lovely blossoms, one saw the most wretched of scenes — men, women and children suffering from leprosy. Numbers were crouching on either side of the road, some were blind, some had no noses, some had hands without fingers, others feet without toes. These poor sufferers displayed their own wretched condition so as to attract the attention of the passers-by to their begging” she writes.13 Almost immediately, a need to hide and regulate the “lepers” of Kumamoto possessed Riddell to the near-exclusion of all else. With determination and leadership somewhat unusual for a Victorian woman, Hannah Riddell raised funds from both expatriates and local Japanese nobility, leased land and built a hospital for 40 “lepers.” On November 12, 1895, Kaishun Hospital opened.

Hannah Riddell |
In Japan, Riddell is regarded as something of a leprosy savior; a woman who lifted “lepers” from a cruel and disordered life on the streets, protected them in her hospital and promoted a scientific approach to the disease and its management. And it is true that she was central to the modernist settlement around leprosy. But no matter how compassionate her approach, Kaishun Hospital and the science behind it were also the opening experiment in a whole techno-scientific project involving leprosy in Japan that was exceptionally unkind, indeed barbaric. “We cannot hope to be beautiful to look at, but we can try to lead beautiful lives”14 one of Riddell’s patients said, but those lives would have to be led with their beauty unwitnessed. Riddell was no scientist, nor was she a technocrat, but her ideas about the science of controlling the contagion of leprosy became part of the solution. Patients at Kaishun Hospital needed government passes to go into Kumamoto, and permission from Hannah Riddell to leave the grounds. Paradoxically, Riddell also insisted that leprosy was hereditary and proselytized her viewpoint among Japanese policymakers who adopted the faulty science without much sign of self-consciousness about the deep contradiction created by putting contagion and genetics together. Riddell put in place methods for keeping genetic transmission of leprosy under control: all Japanese “lepers” were to be prohibited from sexual intercourse and reproduction for two generations.
Riddell drew powerful supporters for her solutions for leprosy in Japan. These men met in 1905 at the elite Bankers’ Club in Tokyo to raise money for Riddell’s work, but the meeting concluded with a call for the government to control and regulate lepers in the ways recommended by Riddell. In 1907, a first version of the Leprosy Prevention Law was promulgated requiring all “lepers” who were without the care and support of non-leprous people to enter and stay in official leprosy sanatoria. The first five of thirteen public leprosy sanatoria were set up in Tokyo, Aomori, Osaka, Kagawa, and Kumamoto; more like prisons than hospitals, they were built in remote places or, when not remote, encircled by high fences or moats. Quickly, Japanese “lepers” were moved into these sanatoria, often by force, and in later years the law was expanded to require all Japanese with leprosy to live in one of the thirteen government institutions and two private sanatoria.
In these places, “lepers” were intensively watched, worked, treated with whatever drugs were made available by Tokyo, disciplined and managed. The institutions themselves were techno-scientific solutions delivered by the modernist settlement in Japan, and so were the patient management policies aggregated around the Leprosy Prevention Law. That the solutions responded to the political problem of how to look modern in Japan was almost entirely elided by a discourse about public safety and duty of care. And the techno-scientific solution concealed the catastrophic effects of the science of leprosy on “lepers” themselves. Castrations and abortions were performed across the sanatorium system: 33 percent of male “lepers” were castrated; 23.6 percent of women were forced to medically terminate their pregnancies.15 Suicide rates were very high. Going beyond the sanatoria became almost impossible for “lepers” and eventually for their non-leprous families. For example, after their father and older brother were deported to a sanatorium, Murata Naoko and Nakamura Hideko were shunned in their Osaka community. Without the income provided by the men of the family and in a community where they were increasingly invisible, the two girls left school before they turned 13 and went to work in another town where their connection to leprosy was unknown.16
Emperor Showa visits Nakakoma Village (now Kai City) in Yamanashi Prefecture, Oct 1947, and discusses the schistosomiasis endemic in the village. Source: World War II Database. |
Into this solution came the consequences of another modernist solution: hepatitis C virus spread by intravenous treatment of schistosomiasis entered the leprosy sanatoria, where it became endemic and caused hundreds of deaths from cirrhosis and liver cancer. It is a long, slow drive from the city of Okayama to the island of Nagashima, not so much because the distance is great but because the island is still out of the way with no railway station, no ferry from a major city, no public bus service, and kilometers from the nearest freeway entrance. There is a bridge to Nagashima now, but until 1988, the crossing was only by boat. This Inland Sea area of Japan is almost always beautiful with slow and silky sea and hundreds of steep green islands in the sun. Nagashima is beautiful too, but it is remote. The government built two leprosy sanatoria here: first Aiseien in 1930, and then Oku-Kōmyō-En in 1938. These days, Aiseien houses both an historical archive meticulously and compassionately managed by Tamura Tomohisa, and about 300 people who used to have leprosy; in 1955 there were 1,701 patients here.
Oku-Kōmyō-En is turning itself into a care facility for aged Japanese, especially those suffering from dementia. It now houses about 200 people who once had leprosy, but in 1960 there were 968 patients. Those who remain housed in these two institutions are old; some have lived their whole lives here. Others left when the leprosy laws changed but returned because life in the mainstream community was not what they had hoped for. Who knows what horrors they saw or experienced? What we do know now is that many of them are infected with hepatitis C virus.
The presence of HCV in the leprosy sanatoria went unseen until the 1990s; the virus was well beyond the ontological horizon until the late 1970s, only suspected for most of the 1980s until a group of researchers working for Chiron Corporation in California detected it in 1989 and techniques for seeing the virus particle, along with tests for the presence of active virus and for counting the amount of virus in the blood stream became available a few years later. In 1996, however, a study of 229 leprosy patients in two leprosy sanatoria showed that 18 percent of them had active HCV infection, very much higher than the percentage of Japanese in the general population positive for HCV.17 Researchers theorized a special comorbidity between leprosy and HCV infection, a possible biological or pathological link between the two diseases, but the story was more complex than that. In 2010, new information about leprosy, HCV and modernity came to light at Oku-Kōmyō-En on Nagashima. Between 1940 and 1980, medical officers at the sanatorium had routinely performed autopsy on almost all of the approximately 1,000 Oku-Kōmyō-En patients who died during those years. At autopsy, they harvested samples of liver tissue. These they preserved using formalin, then archived. The collected tissue samples then remained available for research at the sanatorium pathology archive. Beginning in 2006, they were reviewed, re-sampled and embedded in paraffin for optimal preservation. Around 2008, a team of researchers made two remarkable discoveries about the history of patient deaths at Oku-Kōmyō-En. First, the team found a steep increase in patient deaths caused by cirrhosis of the liver after 1960, and second, it observed an equally sharp increase in patient deaths caused by liver cancer after 1970.

National Sanatorium Oku-Komyo-En |
Seeking to explain the causes of the exceptionally high rates of liver cirrhosis and liver cancer at Oku-Kōmyō-En, the team quickly turned its attention to the liver tissue samples again, this time choosing 48 samples from patients who had died of cirrhosis or liver cancer between 1940 and 1980. Using a microtome and changing its glass blade between each slice, the team cut each liver sample into five micro-slices from which total RNA was extracted. Since chronic HCV infection had been the principal cause of liver cancer in Japan for a number of years, the team tested the samples for genetic remains of hepatitis C virus. HCV has six genotypes, identified by Arabic numerals, and multiple subtypes within each of the six genotypes identified by the Roman alphabet. The research team found HCV-1b and HCV-2a in more than 70 percent of all 48 samples.18 Hepatitis C virus had been killing patients at Oku-Kōmyō-En for decades.
Because the time between initial infection with HCV and full-blown cirrhosis and liver cancer averages between twenty and thirty years, and because cirrhosis and liver cancer were present in samples taken from patients who had died after 1970, the team at first speculated that the virus had been introduced into the leprosy community on Nagashima in the 1940s. But, a subsequent study of the tissue archive by the same researchers revealed three HCV-positive samples of cirrhotic liver tissue from the 1940s.19 This meant that the first patients at Oku-Kōmyō-En to die of diseases caused by HCV infection probably contracted the virus between 1915 and 1925, ten years or so after Hannah Riddell’s solution for the problem posed to modernity by leprosy had been adopted and elaborated by the national government and just a few years after the Eiseika had started mass intravenous injections for schistosomiasis in regions not far from Oku-Kōmyō-En. As Japanese modernity settled for scientific solutions to political problems, and segregated technology and science from society and culture, localized consequences were becoming national with devastating effects for the leprosy community.
In strict epidemiological terms, the HCV infestation at leprosy sanatoria probably came in from the bolus of infections in schistosomiasis communities, and then spread within the sanatoria until between 18 and 25 percent of patients were infected. Yet again the principal technological solution to the health of entire populations (itself a political problem) was at fault: hypodermic delivery systems. Health workers used HCV-contaminated syringes to inject antimony tartrate and Stibnal in schistosomiasis treatment, and HCV-contaminated syringes were almost certainly the main transmission technology in the leprosy sanatoria. Intravenous injections of Chaulmoogra oil (Hydnocarpus wightiana) were a routine, and ineffective, therapy for leprosy, and the first effective drug for leprosy, Promin was also delivered intravenously. Leprosy can also cause severe pain, as did intravenous injection of Chalmoogra oil; intravenous injection of analgesia was a routine treatment for pain in the sanatoria. Disposable syringes were either unknown or not available in these places for much of the 20th century. Tamura Tomohisa, curator of the history museum at National Sanatorium Nagashima Aiseien on the opposite end of the island from National Sanatorium Oku-Kōmyō-En, also suggests that the HCV infection rate was so high not simply because of contaminated syringes but also because Tokyo never allocated budget to the leprosy hospitals sufficient for effective sterilization and/or replacement of syringes and other instruments used in invasive therapies, such as debridement or cutting away of dead flesh around leprous ulcerations.20 Tamura also claims that already low staffing levels at the sanatoria, caused by prejudice and stigma associated with leprosy, were even further reduced by miserly funding from Tokyo and the prefectural governments. In the absence of staff, patients conducted treatments on each other, injecting Chaulmoogra oil and cutting away dead tissue themselves without infection control.21 Both leprosy and schistosomiasis challenged the perfectibility of Japanese modernity and both were subjected to techno-scientific solutions coming from a new public health system. These solutions overlapped. In that overlapping, a new and considerably more formidable threat formed: the chronic hepatitis C infection endemic.
Of course, hepatitis C virus had nowhere to go from the leprosy sanatoria; like its human hosts, it was incarcerated there, but beyond the sanatoria, the modernist settlement in Japan meant that the HCV introduced as a corollary of programs to eradicate schistosomiasis leaked all over Japan between 1940 and 1980, forming a huge bolus of infections that would not be seen until the last years of the 20th century. Yet, once the different parts of this bolus came to light, they could all be tracked back to elements of the modernist settlement and modernization in Japan. Take for example, the story of the Daigo Fukuryū Maru. On March 1, 1954 the United States detonated a hydrogen bomb at Bikini, an atoll of 23 islands circled around a 230 square mile lagoon in the western Pacific region of Micronesia. The explosion turned out to be considerably larger and more powerful than anticipated.
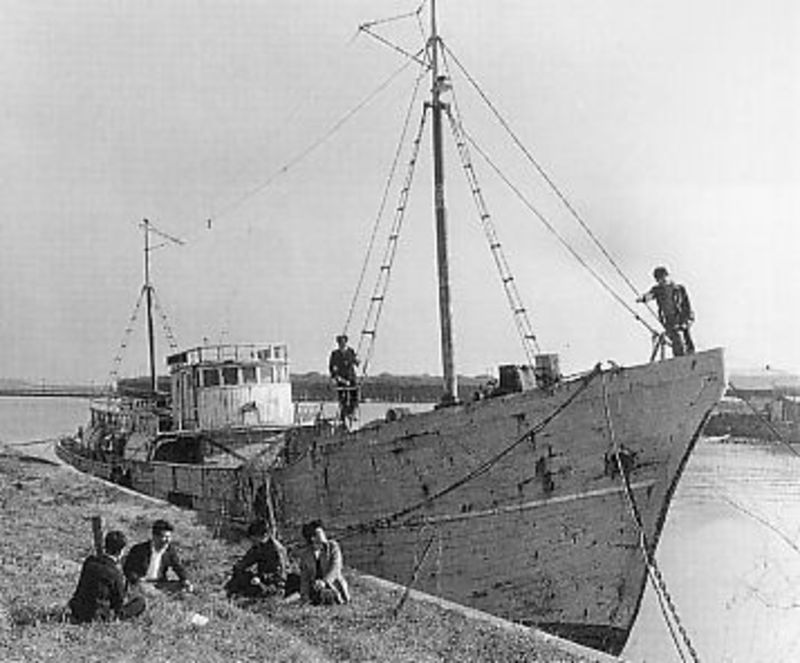
The Daigo Fukuryū Maru shortly before leaving for Bikini Atoll |
Radioactive contamination spread widely in the region and a plume of lethal fallout swept over a Japanese tuna fishing boat trawling about 100 miles east of Bikini: Daigo Fukuryū Maru or Lucky Dragon No. 5. For hours, sandy radioactive ash rained down on the 23 crewmen aboard Daigo Fukuryū Maru. By the next day most of them were ill, nauseated, vomiting, in pain and with inflamed skin: all symptoms of acute radiation sickness. By the time the trawler returned to its homeport at Yaizu in the Shizuoka area, the crew were acutely ill with radiation disease. One died in September 1954. The others were hospitalized, treated, and survived. By 2004, however, more than half of these surviving Daigo Fukuryū Maru crewmen were dead from liver cancer or cirrhosis caused by chronic HCV infection. At first, their diseases were put down to alcohol abuse, but by 2010 it was clear that Japanese doctors had used blood transfusions to treat the leukopenia caused by the crewmen’s radiation sickness and that the donated blood had been contaminated with hepatitis C virus.22 As Dr. Akashi Makoto, director of Japan’s National Institute of Radiological Sciences, remarks, “Exposure to American nuclear fallout and exposure to HCV are not directly tied, but the hepatitis C virus infections originated as part of the Lucky Dragon No. 5 incident.”23
Akashi is on the right track here: the HCV infections of the Daigo Fukuryū Maru crewmen do indeed refer us to the Cold War. Beyond its conflict of ideas, the Cold War was a battle between two infrastructures. Infrastructure provides the wide-ranging techno-scientific modernist solution to the fragmentation of “macro, meso, and micro scales of time, space, and social organization” in modern societies; it forms “the stable foundation of modern social worlds.”24 Yet, the Daigo Fukuryū Maru HCV infections and deaths were also consequences of the late Meiji and Taishō modernist settlement within Japan which had blindly delivered an HCV epidemic in its solution to schistosomiasis, itself both a clinical and a political problem. From the schistosomiasis solution, HCV entered the blood supply of postwar Japan. But the trajectory of the virus from prewar schistosomiasis programs to the blood banks and plasma processing factories of Japan in the 1950s, 1960s, and 1970s passed through another techno-scientific modernist solution to a political problem that amplified the endemic spread of the virus: methamphetamine.
Formation of a modern research and development scientific community policed by principles of shared assumptions, universal methods, replicable results and empirically observable outcomes was a vital part of Japan’s modernization: without it there could have been no modernist settlement. The modern science of chemistry and its technological relative, pharmaceutical research and development, were core parts of the settlement.

Nagai Nagayoshi: Father of modern chemistry in Japan and discoverer of methamphetamine |
Nagai Nagayoshi was a leading figure in the formation of chemical sciences and pharmaceutical technologies in Japan: he was also the discoverer of methamphetamine. Like Sensai Nagayo, the founder of public health in Japan, Nagai studied rangaku (Dutch Learning) and spent time in Nagasaki in the 1850s where he built connections with men like Itō Hirobumi and Ōkubo Toshimichi, who would soon dominate Japan’s modernization. Like Sensai, Nagai also spent time in Germany during the 1870s. He studied at the University of Berlin, now Humboldt University of Berlin. Back in Japan, Nagai bore overall responsibility for establishing and developing modern chemistry; for Nagai, modernity was to be found in the universalism of organic chemistry and in the uses to which it could be put to improve Japan. As professor of chemistry at Tokyo Imperial University, he began a modern chemical analysis of ephedra herba, a plant with a long history of use in both Chinese traditional medicine and its Japanese version, kanpō. In 1888, he discovered the alkaloid, ephedrine hydrochloride, which would be synthesized into methamphetamine in 1893 and into crystalline meth by Ogata Akira in 1919.25
For several decades, methamphetamine languished. To begin with, its only use was as an agent to contract chronically over-dilated pupils in cases of mydriasis, or “blown pupil.” Then, after World War I, the drug became commercially viable as an injectable broncho-dilating treatment for asthmatics26 but as Japan’s military commitments in China expanded, and after the war with the United States began in December 1941, methamphetamine became a scientific solution to the political problem of imperial preservation and protection of the Japanese state. Dai-Nippon Seiyaku Company sold oral and injectable forms of methamphetamine under the trade name of Philopon (hiropon) to keep Japanese fighting and producing for the empire and the war to defend it. As Jeffrey Alexander remarks: “during the Second World War Japan’s military government came to consider it [Philopon] a safe, effective stimulant for tired pilots, signal corpsmen, and munitions workers, and it ordered a swift and dramatic increase in production.”27
After surrender the political problem solved by methamphetamine changed. Now the stimulant was used to resolve the anxieties, trauma, and exhaustion produced by the political problem of defeat, loss of sovereignty and living in the ruins of war under American occupation. By the late 1940s more than 20 Japanese drug companies produced and marketed methamphetamine for relief of hypotension, fatigue and sluggishness.28 After manufacture and sale of methamphetamine in powder or tablet form were banned in 1949, manufacturers turned to injectable solutions. Miriam Kingsberg reports that use of the stimulant was very high and she gives as evidence the perhaps not very exemplary story of twenty-year-old Sakemaki Shūkichi who was charged with the murder of a young girl while under the influence of methamphetamine in 1954: “At the time of the murder, Sakemaki had been injecting himself with twenty to thirty ampoules of hiropon (Philopon), a type of methamphetamine, daily for two years” she writes.29 And although Sakemaki’s use may have been on the high end of the national methamphetamine usage scale, intense use of methamphetamine delivered intravenously was happening all over Japan.
Injecting Philopon (hiropon). Source: Shashin Kōhō Photo Bulletin] May, 1954 |
Inevitably, the legal use of intravenously delivered methamphetamine to solve battle readiness, worker productivity, exhaustion and war trauma opened up a way for the relatively contained boluses of HCV infection around the schistosomiasis communities to spread. Even after the government passed an Amphetamines Control Law in 1951, widespread use of methamphetamine did not stop. The strict separation of science from society, central to the epistemological structure of the modernist settlement, now disintegrated. The science of making crystalline methamphetamine went into the hands of criminal organizations. Meth labs using base compound smuggled in from Macao and Hong Kong and run by criminal enterprises proliferated in Japanese cities. What is more, one of the core technological devices for modernization of health, the hypodermic syringe, had already escaped the scientific arena and become popular technology: by the time methamphetamine was made illegal, Japanese were well-accustomed to injecting themselves at home with vitamins and other drugs, and hypodermic syringes and needles were available for legal purchase at every corner drug store.30 Injection of methamphetamine continued.
Persistent intravenous use of methamphetamine after criminalization spread hepatitis C virus even further in Japan; so far and so thickly that it entered the postwar blood supply. This final stage of the epidemiology could have happened earlier had blood been scientized by modernity earlier than it was. But in Japan’s modernist settlement, the mystical significance of blood was slow to cross the epistemological gulf between culture and science. Blood letting had been an untroubling part of Tokugawa era medicine for centuries, but even though Drs. Gotō Shichirō and Shiota Hiroshige had separately witnessed the almost miraculous effects of blood transfusion on wounded soldiers in Europe in 1916 and had separately brought transfusion equipment back to Japan, the technology triggered some resistance in Japan and failed to catch on. In February 1919, Gotō transfused 300 ml of blood into a patient during thoracic surgery; in June of the same year, Shiota performed transfusion of 200 ml of blood into a patient with uterine fibroids.31 Other transfusions followed, including one in 1930 on Prime Minister Hamaguchi Osachi who had been shot at Tokyo Station in an assassination attempt.
By the time of Japan’s attack on Pearl Harbor and the beginning of the Pacific War, both the United States and the European powers had come to regard blood as vital strategic materiel. The problems of transporting blood supplies to the frontline and to preservation had largely been solved, partly through development of plasma powder. As a result, blood supply and transfusion techniques played a significant role in the Allied victory but, although Japanese scientists found their own way to powdered plasma, there was no donor base from which to obtain large quantities of whole blood in Japan and by the time the new technology became available, Japan’s supply lines to its far flung fronts were too unreliable for the technology to reach troops. After the war, however, a rapidly expanding and highly profitable business in collection of blood, and supply of whole blood and plasma products for use in clinical situations and in new drug formulations, emerged. At the center of this new business and its new products were both American techniques for managing blood and making blood products, as well as technological and scientific solutions worked out at or abstracted from the work of the infamous Unit 731 laboratories outside the Chinese city of Harbin, then in the Japanese puppet state of Manchukuo, during the war. Dr. Naitō Ryōichi developed freeze drying technology for use in experiments on Chinese prisoners and POWs at Unit 731 headquarters there;32 after the war he used the same technology to start a blood and blood products company that grew into a multi-billion dollar transnational business: Green Cross. Kitano Masuji, another member of the Unit 731 team managed Green Cross for Naitō. Like other Unit 731 scientists, Kitano and Naitō were not prosecuted for war crimes by the United States after the war; data from their experiments on human subjects were valuable bargaining chips.
It is easy now to forget that until the late 1960s the Japanese people were not rich. In the first 10 years after defeat, they were especially poor, often desperate. Green Cross and other blood collection and processing businesses in Japan paid for donations of whole blood, and giving blood became quite a business in itself. By the 1980s, Japan used more blood and blood products than any other country. Demand outstripped supply.33 Green Cross and the Japanese Red Cross Society had to import blood. Screening was rudimentary, and in any case, lethal blood borne viruses like hepatitis C virus were almost unknown. The HCV endemic in the schistosomiasis communities and among the vast numbers of people who injected methamphetamine, along with HCV imported in blood from abroad, entered the national blood supply.

Cartoon depicting long-term effects of HCV infection on the liver. Source. |
More than 50 percent of Japanese transfused with blood developed post-transfusion hepatitis. 34 Although the government was aware of the problem it did not act until the news of Edwin Reischauer’s post-transfusion hepatitis caused such a scandal that lawmakers had no choice but to change the system. Paid blood donation was phased out beginning in 1964; screening for hepatitis B antigen was introduced in 1972.
Even so, Japanese doctors soon discovered what their colleagues in the United States already knew: screening for hepatitis A and hepatitis B viruses was not eradicating post-transfusion hepatitis, but it was not until 1989 that HCV was detected and a test became possible. In the meantime, the giant business in blood and blood products infected millions of Japanese with hepatitis C virus: the endemic enabled by development of a public health system as part of the modernist settlement and begun with the schistosomiasis eradication programs in the 1920s and 1930s, then expanded by intravenous use of methamphetamines during the war and after, now reached a kind of epidemiological apotheosis. The disease once confined to rural communities in marshy areas and to “lepers” in institutions could now be found across the nation: between 2 and 3 million Japanese presently live with this most modern of viruses; millions more are affected by it as family members, coworkers, healthcare professionals.35
In May 1988, after giving birth to her first son at a hospital in the city of Ise, Kuno Ikuko began to bleed. Her obstetrician gave Kuno fibrinogen, a Green Cross blood-clotting drug manufactured using human blood products. Kuno became ill. Her skin turned yellow not long after her treatment with the coagulant, and although the jaundice left her, she began to feel chronically ill. In the early 1990s, Kuno was tested and told she had chronic hepatitis C infection. As an infant in Nagasaki, Fukuda Eriko was given Christmassin, a Green Cross clotting agent made from human blood products. At the age of 20, Ms. Fukuda learned she had chronic HCV infection; the blood products used to manufacture Christmassin had been contaminated with HCV. Kawada Ryūhei was born hemophiliac. At the age of 10 his mother told him that the Green Cross blood-clotting drugs he had been using to keep himself alive had given him both HIV and HCV. Watanabe Ken, cinema actor and star of The Last Samurai, has chronic HCV infection. The great enka singer, Misora Hibari had HCV infection. Kōno Yōhei, a former Deputy Prime Minister and president of the Liberal Democratic Party, has hepatitis C virus and underwent a liver transplant in 2002. Green Cross, which had already been held accountable for HIV infections caused by its blood products, now faced a second scandal to do with hepatitis C virus: the company had failed to screen for the hepatitis B antigen, which was a predictor of HCV at a time before 1989 when hepatitis C had not yet been discovered, but was thought to exist and to be responsible for millions of cases of what was then called non-A non-B hepatitis.
*******
Modernity and its settlement were always bricolage in Japan: ideas and techniques from the pre-1868 ancien regime not only persisted but were networked into modernity alongside, but epistemologically divided from, the new. And, although Japan is usually considered a latecomer to modernity, its modernizers acted with extraordinary alacrity to settle modern science and technology for Japan and to set them off together from any admitted transactions with any parts of the modernist settlement other than economics: science and technology were heavily linked to economic progress but were purified of culture and politics. Less than 20 years after the Meiji Restoration, a modern, scientific public health machine had been started, and indigenous clinical sciences, chemistry and pharmaceutical technologies had begun to take shape. These too, were epistemologically divorced from other arenas of the modernist settlement, but were nonetheless used to provide solutions both formal and informal to political problems: national hygiene indexed modernity; infection control and disease eradication provided an effective workforce for a modern state; scientific incarceration removed the ancient blight of leprosy from sight; chemicals helped extend the empire, preserve the sovereignty of the militaristic state, and then made the postwar world possible in existential terms for many. From these solutions delivered by the quick and effective modernist settlement in science came Japan’s early hepatitis C virus endemic, which stands today as both a challenge to Japan’s 21st century modernist settlement and as a symbol of modernist settlements made in Japan’s past.
Acknowledgements
This essay owes its existence to Tamura Tomohisa, curator of the history museum at National Sanatorium Nagashima Aiseien, and to Professor Muta Orie. Thank you.
Recommended citation: Vivian Blaxell, “Yellow Blood: Hepatitis C and the Modernist Settlement in Japan.”, The Asia-Pacific Journal: Japan Focus, Vol. 12, Issue 18, No. 1, May 5, 2014.
Notes
1 Quoted in George R. Packard, Edwin O. Reischauer and the American Discovery of Japan. (New York: Columbia University Press, 2010), p. 205. My account of the assassination attempt is also taken from Packard.
2 Melissa M. Center and Ahmedin Jemal, “International Trends in Liver Cancer Incidence Rates.” Cancer Epidemiology, Biomarkers and Prevention, 2011, Vol. 20, No. 11, pp. 2362 – 2368.
3 Iwao Ikai, Masatoshi Kudo, Shigeki Arii, Masao Omata, Masamichi Kojiro, Michiie Sakamoto, Kenichi Takayasu, Norio Hayashi, Masatoshi Makuuchi, Yutaka Matsuyama & Morito Monden, “Report of the 18th follow-up survey of primary liver cancer in Japan.” Hepatology Research, 2010, Vol. 40, pp. 1043–1059.
4 Bruno Latour, We have never been Modern, translated by Catherine Porter, (Cambridge, MA; Harvard University Press, 1993), Location 2666 in Kindle edition.
5 Quoted in Ann Bowman Janetta, “From Physician to Bureaucrat: The Case of Nagayo Sensai” in Helen Hardacre and Adam Kern, editors, New Directions in the Study of Meiji Japan. Brill’s Japanese Studies Library, Book 6 (Leiden, Boston & Tokyo: Brill, 1997), p. 159.
6 Nagasaki University School of Pharmaceutical Sciences, Kusuri no rekishi, Nagasaki yakugakushi no kenkyū, Daisanshō kindai yakugaku no teichakuki. Iryō – Eiseigyōseisei no sōshisha: Nagayo Sensai. [The history of pharmaceuticals, Research into pharmaceutical science history. Chapter 3: The period of establishment of pharmaceutical sciences. Nagayo Sensai: Founder of the medical care and public health systems.] Viewed 04/13/2014.
7 M. Mizokami, Y. Tanaka, Y. Miyakawa, “Spread times of hepatitis C virus estimated by the molecular clock differ among Japan, the United States and Egypt in reflection of their distinct socioeconomic backgrounds.” Intervirology, Vol. 49, 2006, pp. 28–36.
8 Yasuhito Tanaka, Kousuke Hanada, Etsuro Orito, Yoshihiro Akahane, Kazuaki Chayama, Hiroshi Yoshizawa, Michio Sata, Nobuo Ohta, Yuzo Miyakawa, Takashi Gojobori & Masashi Mizokami, “Molecular evolutionary analyses implicate injection treatment for schistosomiasis in the initial hepatitis C epidemics in Japan.” Journal of Hepatolology, Vol. 42, No. 1, January 2006, pp. 47-53.
9 The term “leper” to name people with Hansen’s Disease is considered pejorative in both Japan and elsewhere these days. But “leper” or the Japanese equivalent, raibyōkanja, was the language of the times described in this essay. “People with Hansen’s Disease” is language adopted in the latter years of the 20th century. I use “leper” in inverted commas to be at once historically accurate and to acknowledge the stigmatizing power of the word.
10 I am thinking here of the beauty found in asymmetrical, rough, and accidentally imperfect ceramics, or of Mishima Yukio’s aestheticization of war and violence. Late one spring night many years ago, I was walking with a Sōtō Zen monk through the groves of cherry trees lining the banks of the Ōi River at Arashiyama. The cherry trees were in full bloom and beneath them lay great middens of trash left by revelers. I commented on the ugliness of it. “However,” my monastic companion said, “Is not the trash beautiful too, for it forces the eye to travel up to the blossoms and into the night sky.”
11 Susan L. Burns, “From ‘leper villages’ to leprosaria: Public health, nationalism and the culture of exclusion in Japan” in Carolyn Strange and Alison Bashford, editors, Isolation: Places and practices of exclusion. (London & New York: Routledge, 2003), p. 100.
12 William Ng, “The Literary Works of Hansen’s Disease Patients in Japan.” International Journal of Dermatology, Vol. 49, Issue 4, April 2010, p. 462.
13 Quoted in Tobumatsu Jingo, Hannah Riddell: Known in Japan as “The mother of lepers. Project Canterbury. Viewed December 20, 2012.
14 Quoted in Julia Boyd, 1996. Kindle Location 2018.
15 Tokie Takahashi, “Taking Social Responsibility for the Legal Isolation of Patients with Hansen’s Disease.” Essays 2006. Nagoya Women’s Studies Research Group, 2006.
16 Fukuoka Yasunori and Kurosaka Ai, “Zettai ni, kokkara ugoku monka to – chichi to ane ga hansen byou ryouyoujo ni shuyousareta shimai no katari” [No way are we leaving here – Sisters whose father and older brother had been put in a leper sanatorium tell their story] Nihon Ajia Kenkyuu [Japan Asia Research, No. 8., March, 2011.
17 Katsushi Egawa, Tomo Yukawa, Shoichi Arakawa, Takeshi Tanaka, Fumio Tsuda, Hiroaki Okamoto, Yuzo Miyakawa and Makoto Mayumi, “Hepatitis C virus antibody, viral RNA and genotypes in leprous patients in Japan.” Journal of Hepatology, Vol. 196, No. 24, pp. 397-402.
18 Kazuya Shiogama, Hidemi Teramoto, Yukiko Morita, Yasuyoshi Mizutani, Ryoichi Shimomura, Ken-ichi Inada, Toshio Kamahora, Masanao Makino, and Yutaka Tsutsumi, “Hepatitis C Virus Infection in a Japanese Leprosy Sanatorium for the Past 67 Years” Journal of Medical Virology, Vol. 82, 2010, pp. 556–561.
19 Hidemi Teramoto, Kazuya Shiogama, Yasuyoshi Mizutani, Ken-ichi Inada, Toshio Kamahora, Masanao Makino and Yutaka Tsutsumi, “Molecular Epidemiology of a Hepatitis C Virus Outbreak in a Leprosy Sanatorium in Japan.” Journal of Clinical Microbiology, Vol. 49, No. 9, Sept. 2011, pp. 3358–3360.
20 Personal communication via email, 12/28/2012.
21 Personal communication at Aiseien, 27/05/2013
22 Juntendo University Shizuoka Hospital, Faculty of Medicine, Shiigatakanen uirusu wo kiru! [Kill HCV!]. Viewed June 27, 2013.
23 Quoted in Bikini jiken – hanseiki no kokuin: 5/ tairyou yuketsu de kanenhasshou [The Bikini Incident – Impressions of half a century: No. 5/ Major blood transfusions and outbreak of hepatitis] Mainichi Shimbun, March 5, 2004. Viewed June 27, 2013.
24 Paul N. Edwards, “Infrastructure and Modernity: Force, Time, and Social Organization in the History of Sociotechnical Systems” in Thomas J. Misa, Philip Brey, Andrew Feenberg, editors, Modernity and Technology. (Cambridge, MA: The MIT Press, 2004), p. 186.
25 Sato Akihiko, “Methamphetamine use in Japan after the Second World War: Transformation of Narratives.” Contemporary Drug Problems, Vol. 35, Winter 2008, pp. 717-746.
26 Miriam Kingsberg, “Methamphetamine Solution: Drugs and the Reconstruction of Nation in Postwar Japan.” Journal of Asian Studies, Vol. 72, No. 1, 2013, pp. 141-162.
27 Jeffrey W. Alexander, “Japan’s hiropon panic: Resident non-Japanese and the 1950s meth crisis.” International Journal of Drug Policy.May 2013, Vol. 24, No. 3, p.
239.
28 Kazuya Shiogama, Hidemi Teramoto, et al, 2010, p. 561.
29 Kingsberg, 2013.
30 Alexander, 2013, pp. 238-43.
31 Saito Katsuhiro, “Hiroshige Shiota.”Nihon Ishikai Zasshi [Journal of the Japan Medical Association], 1965, Vol. 53, No. 1439.
32 Nishiyama Katsuo, “’15-nen sensō’ e no Nihon no igaku iryō no katan no kaimei ni tsuite” [Participation of Japanese medicine in the 15 Year War], Shakai igaku kenkyū Social Medicine Research 2009, Vol. 26, No. 2, pp. 11-26.
33 S. Sekiguchi, “The Impact of Blood Substitutes on the Blood Program.” E. Tsuchida, editor, Blood Substitutes: Present and Future Perspectives. (Amsterdam: Elsevier Science, 1998), pp. 383.
34 Hobyung Chung, Taisuke Ueda, Masatoshi Kudo, “Changing Trends in Hepatitis C Infection over the Past 50 Years in Japan.” Intervirology, 2010, Vol.53, pp. 39–43.
35 Gordon G. Liu; Marco da Costa DiBonaventura; Yong Yuan; Jan-Samuel Wagner; Gilbert J. L’Italien; Paul Langley & Isao Kamae, “Burden of Viral Hepatitis C in Japan: A Propensity Analysis of Patient Outcomes.” Poster session at the 21st Conference of the Asian Pacific Association for the Study of the Liver, APASL 2011, Bangkok, Thailand, February 17-20, 2011. Available here. Retrieved May 3, 2014.