Migrant Health in Japan: Safety-Net Policies and Advocates’ Policy Solutions
Neal S. Parikh
Abstract
Japanese migrant policy prioritizes immigration control over migrant rights and welfare, which has clear consequences for migrant healthcare. A literature review and interviews of migrant healthcare advocates revealed that disadvantaged migrant groups have poor health and face barriers in accessing mainstream healthcare, particularly for emergency, HIV/AIDS and maternal and child care. Advocates fashion a provisional safety net from existing policies to connect migrants with essential care, but this approach is of limited effectiveness. Policy solutions and relevant advocate opinion are considered in light of the failure of existing policies to meet uninsured migrants’ healthcare needs.
Keywords
Safety net, migrant healthcare, migrant health policy, advocacy
Abbreviations and Acronyms
MLHW Ministry of Labor, Health and Welfare; NHI National Health Insurance; EHI Employee Health Insurance; MCH Maternal and Child Healthcare; JAR Japanese Association of Refugees; SHARE Services for the Health in Asian and African Regions
Introduction
Migrants with restricted immigration status, such as those without official visas, without current visas, and without visas that allow free employment, are a vulnerable population that faces limited healthcare access (1,2). In this context, many developed migrant-receiving Western nations like those of the European Union and North America have established safety-nets that meet migrants’ healthcare needs to varying degrees (3,4). According to the Institute of Medicine definition that is widely used in the American context, safety-net providers “organize and deliver a significant level of health care and other health-related services to uninsured…and other vulnerable patients” (3). In countries with universal healthcare or public health insurance schemes that are limited to citizens and migrants with restricted visa categories, some migrants fall into the vulnerable patient category and thus require a safety net. Health policies, laws and international covenants establish safety-net systems of such providers to extend varying levels of care to said vulnerable patient populations, as is the case in most EU nations.
While EU member nation migrant health policies are diverse, a brief description of German and Italian policy allows for contextualization of the situation in Japan (4,5,6,7). On the migrant-friendly end of the spectrum, Italy provides universal coverage and extends partially or fully subsidized emergency care, primary care, infectious disease care, including that for HIV/AIDS, and MCH to all migrants, including undocumented migrants, who obtain an anonymous “STP code”. In practice, care accessibility varies with medical institution, region and NGO presence and migrants, like Italian citizens, must pay a potentially prohibitive “ticket” fee for services; however, access to essential care for the vulnerable migrant population, and hence a safety net, has been established. Germany, in contrast, ultimately provides very limited safety-net coverage to irregular migrants – undocumented migrants and asylum seekers. On one hand, the Asylum Seekers Benefits Law, together with the Penal Code and Law for Infectious Diseases, entitles refugees, asylum seekers, persons holding a Duldung or temporary deportation hold and undocumented migrants to, at minimum, emergency care, limited infectious disease care and pre- and post-natal care. Undocumented women and their infants are eligible for a Duldung from six weeks prior to delivery to eight weeks after, as are undocumented migrants undergoing treatment for Tuberculosis and HIV/AIDS. This safety-net is handicapped by limiting policies that, for example, compel public authorities like the welfare officials who reimburse providers for undocumented migrant care to report irregular migrants for possible deportation and that criminalize routinely assisting irregular migrants. Additionally, upon expiration of a Duldung, the migrant is subject to deportation. Hence, in practice, conflicting policies severely limit the utility of the safety net in Germany.
In principle, however, most developed Western nations guarantee access to emergency healthcare and some level of infectious disease care and protect the welfare of women and children regardless of residential status. EU nations are signatories of Article 12 of the International Covenant on Economic, Social and Cultural Rights and the non-binding Charter of Fundamental Rights of the European Union, which affirms “the right of everyone to access to preventive health care and the right to benefit from medical treatment” (4). While some EU nations neglect or override components of these conventions, the basic principles therein are unadulterated as is reflected in the various nation-specific policies that seek to enforce the principles of these conventions by affirming, at minimum, the right of access to emergency care and limited infectious disease and MCH.
Japan is a developed nation with a relatively limited migrant population – 1.69% of its total population is non-Japanese (8). Japanese immigration policy prioritizes migrant control over migrant rights (9), and this policy dynamic manifests itself in the nearly nonexistent healthcare safety net and the resulting transfer of responsibility to NGOs and civil groups. Migrants’ limited healthcare access in Japan (10), stemming from their exclusion from Japan’s public health insurance schemes and the inability of Japan’s provisional safety-net policies to serve migrants’ needs, has elicited a societal response that seeks to fill the gaps left by inadequate policy while offering and often advocating for policy solutions (11).
Investigations of Japanese migrant health and policy are rooted in humanities and social science perspectives (12,13,14,15,16) and have yet to offer a comprehensive evaluation of Japanese health policy and advocates’ policy solutions in the context of healthcare safety nets. This article surveys key policies relevant to the healthcare of disadvantaged migrants in Japan and argues, based on migrant health data and advocate interviews1, that they do not meet migrants’ needs and do not form a reliable safety net. However, these policies could form a comprehensive safety net through incorporation of advocates’ policy solutions.
|
* Estimated as total of Brazilian and Peruvian national long-term residents and Brazilian spouses and children of Japanese nationals. |
The author limited this study to issues of emergency care, infectious disease and maternal and child healthcare (MCH) to mirror the priorities of Japanese advocates and researchers. Additionally, while safety nets serve all residents with limited healthcare access, this article focuses on Japan’s disadvantaged migrants2: visa overstayers (overstayers), asylum seekers, Latin Americans of Japanese descent (Nikkeijin), and foreign trainees and technical interns (trainees). Nikkeijin, Latin Americans of Japanese descent to the third generation, and their spouses receive renewable long-term visas and live and work freely in Japan. Foreign trainees enter Japan to acquire skills, knowledge or technology and transfer these to developing countries. After initial training, they labor in Japanese companies and can extend their stays as technical interns. Together, they meet many of Japan’s “3D” – dirty, dangerous and dull – labor needs (12). Lastly, according to the Japanese Association for Refugees (JAR), refugee decisions take approximately two years, so asylum-seekers who enter with three-month tourist visas and are denied provisional stay visas upon refugee application become overstayers in waiting (17). Table 1 provides population figures for these migrants. Aggressive deportation has nearly halved the overstayer population since 2004 (18), and asylum-seekers nearly doubled from 2007 to 2008 (19).
Exclusion from Mainstream Healthcare
The Japanese healthcare system consists of employees’ health insurance (EHI), guaranteed to employed individuals and dependents, and national health insurance (NHI), available to the self-employed, retired and their dependents. The EHI premium is split between the employee and employer; NHI policyholders are responsible for the entire premium. Together, these programs provide healthcare access to most people in Japan, but access to both is limited for many migrants (12).
Although EHI is legally guaranteed to most employees, many firms that employ overstayers, Nikkeijin and trainees violate labor standards and discourage enrollment to avoid paying the employer’s half of the premium. Additionally, EHI is coupled with pension, which discourages EHI enrollment for short-term migrants; migrants leaving the country receive lump sum refunds of employee pension contributions, but the refund is limited to six-month increments totaling a maximum of three years. Though many Nikkeijin enjoy relatively stable employment in relatively established companies, their EHI enrollment rate is low – 28.3% in one city – and varies by municipality (20). After initial training, trainees are eligible for insurance; however, Takayama Toshio, a social worker and migrant health advocate since 1987, contends that trainees, too, are often uninsured. He referenced a case in which he was recently involved: “I had a person come in recently – an uninsured trainee – I told him he could get health insurance since he had a visa, but he didn’t understand the system and nobody had told him. The agency who brought him to Japan just introduced him to a company and didn’t confirm whether he was enrolled in health insurance” (21). As for NHI, Ministry of Health, Labor and Welfare (MHLW) policy officially excludes those residing in Japan for less than one year, thereby effectively excluding overstayers, including those who enter Japan on three-month tourist visas, which includes many asylum-seekers (11,12). Additionally, while Nikkeijin without EHI officially can enroll in NHI (22), Dr. Sawada Takashi, a longtime physician advocate for migrant health, has found many municipalities he has interacted with to be unaware of this policy (23). Thus, these migrants groups, whether officially or effectively excluded from enrollment, need a safety net in times of urgent medical need.
Unreliable, Provisional Safety-net Policies
A major healthcare barrier for uninsured migrants in Japan is cost. Many migrants delay seeking care until their condition deteriorates, by which point the cost of care has increased. Hospitals caring for such patients are often left with unpaid medical bills and thus financial burdens (11). Additionally, Dr. Sawada reports that public national hospitals, though previously more accommodating, have become less willing to treat migrants because the national government has pushed for hospital financial independence and profitability since 2000 (23). Catherine Campbell of the National Union of General Workers Tokyo Nambu noted that patients are occasionally retroactively enrolled in insurance programs at the point of care (24), but this solution is meaningful only for eligible migrants and only when the cost of care exceeds the retroactive premium.
Hence, in most cases, three policies purport to address the medical cost issue. These policies, along with other relevant policies, are listed in Table 2 (22,25,26). The Livelihood Protection program previously covered expenses for uninsured migrants facing serious health issues; however, overstayers and short-term visa holders have been ineligible since 1990 (12). Advocates, including Mr. Takayama, have since successfully engaged some local governments to reinstate the once dormant Travelers’ Law and create reimbursement programs, both of which reimburse hospitals for services provided. Though reimbursement policies could secure emergency care access for migrants, limited geographical availability, budgets and healthcare provider awareness reduce their effectiveness. The Travelers’ Law is also funded for migrant use in only a few prefectures (22,27).
The remaining policies are inadequate in coverage, availability or implementation. The Infectious Disease Law guarantees Tuberculosis treatment but not HIV/AIDS care. MCH policies guarantee access to specified services, but local governments have discretion in providing financial support, which ultimately limits access to services like hospitalized birth and urgent surgery (25). Moreover, local governments inconsistently implement these MCH policies and do not actively promote programs to migrant women, who otherwise are otherwise unaware of their existence (25,28). Finally, though the MLHW allows provision of urgent care to all residents, no current policy formally mandates it (29). As a result, hospitals are not held legally accountable for denying urgent care and are thus left to potentially prioritize financial concerns.
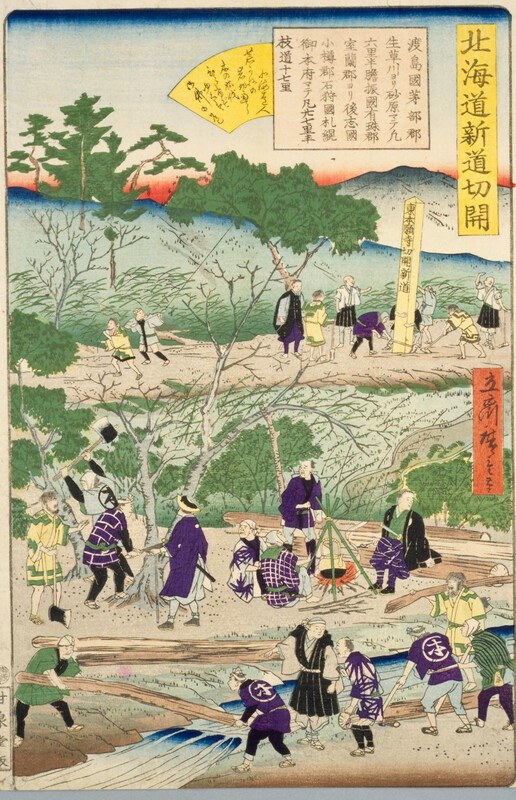
|
The TB prevention chest X-ray mobile unit sits parked outside a free health consultation in Tokyo. |
These policy limitations hinder advocates in their attempts to connect migrants with healthcare. For example, Dr. Sawada explained that the Tertiary-Level Emergency Care Unpaid Bill Reimbursement program is valid only at tertiary-level hospitals, which provide trauma and other advanced care, and is thus usually only applicable to a few cases of trauma care for migrants. Likewise, while JAR utilizes the Free or Reduced Cost Medical Treatment System to connect asylum-seekers with needed care, Dr. Sawada has found implementation rare; he knew of only three hospitals nationwide that make this program available (23). Also, Workmen’s Accident Compensation Insurance is legally mandated for employees, but advocate intervention is sometimes necessary for victims of workplace injuries or illnesses to receive due compensation. Murayama Satoshi, Chairman of the Executive Board of the Kanagawa City Union and a longtime migrant advocate, asserted that labor union intervention is necessary: “It is being left to labor unions because if they [MLHW] were to take care of it universally, it would become expensive – the labor costs would go up” (30).
The existing literature and interviews lead to the conclusion that the safety net that results from described policies is merely provisional in that policy utilization usually requires case-by-case advocate intervention by NGOs like SHARE and JAR. Moreover, the safety net is unreliable; advocates irregularly succeed in securing limited, essential care for uninsured migrants due to inadequate safety-net policy.
Migrant Health
Available migrant health data demonstrates that migrants have unmet emergency care, infectious disease care and MCH needs. Data from NGO-sponsored free health consultations in the Tokyo and Nagano areas provide a general picture of disadvantaged migrant health. 1991-2000 Tokyo-area health consultation data for 2370 migrants showed that Body Mass Index, a measure that relates body weight to height, blood pressure and blood glucose readings were significantly higher for many migrant groups than for their Japanese counterparts (31). Nagano data are similar, though they, unlike Tokyo data, also partially represented Nikkeijin (32). The Nagano study noted the prevalence of preventable and treatable chronic conditions: high blood pressure – 21%; high cholesterol – 20%. Both studies reveal inadequate healthcare access and indicate that migrants face high rates of various chronic illnesses and risk factors that can require emergency care if left untreated.
Two recent cases illustrate limited emergency care and HIV/AIDS care access: two uninsured, overstayer Thai women tested HIV+ and had brain abscesses (33). Both were initially denied urgent care due to their inability to pay and their undocumented visa status, and doctors encouraged repatriation. Ultimately, after repatriation, one woman died and the other was disabled. Such cases are common; advocates like Dr. Sawada and Lee Sangnim of SHARE routinely assist migrants without access to emergency care. Dr. Sawada recalled a case in which a doctor, under pressure from the hospital administration, wrongfully discharged a heart attack patient requiring essential care because she was unable to pay. Dr. Sawada intervened and pressed the hospital to provide care (23). Ms. Lee recounted a case in which a diabetic patient entering diabetic coma was rushed to the hospital by ambulance and was refused care: “He eventually lost consciousness there. The hospital was worried about its accounting to the extent that it let a patient lose consciousness” (34). Given this context, one can understand why Africa Japan Forum (AJF), in addition to SHARE, compile information about hospitals in migrant-sending nations; sometimes the reality is such that the most an advocate can do is arrange post-repatriation care. Inaba Masaki, International and Domestic Health Program Director of AJF, explained, “for HIV, if someone wants to return home, we help them by connecting them with help groups and hospitals at home” (35). Additionally, asylum-seekers regularly utilize JAR’s independent emergency fund for urgent care, the existence of which underscores uninsured migrants’ limited healthcare access (17).
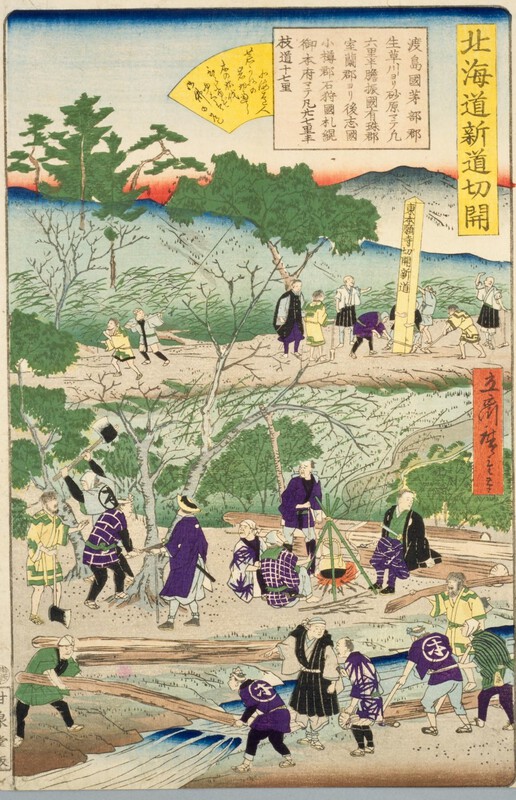
|
SHARE provides free health consultation and health education to migrants during a festival at a Thai temple near Tokyo. |
Migrants in Japan have higher TB and HIV/AIDS incidences than their Japanese counterparts. The 2007 foreign national TB incidence was double that of Japanese nationals (36). Policy makers acknowledge the high TB incidence and have responded with migrant-specific programs. Treatment is publicly financed and detection is facilitated by screenings during free health consultations and at Japanese-language schools; local municipalities often cosponsor the free health consultations in their area (37). Shinjuku, a Tokyo ward with many migrants, created a migrant-specific Directly Observed Treatment Short course (DOTS) treatment program to improve adherence to treatment (37). Additionally, Tokyo (34) and Kanagawa Prefecture (38) have medical interpreter programs that serve migrant TB patients.
In contrast to the TB situation, a policy response to the high migrant HIV/AIDS rate – over 10% of reported cases – has been slow to come (39). Blood test results, specifically low CD4 counts, at first examination suggest that HIV is detected late in disadvantaged migrants, especially in uninsured migrants (40). This study also revealed that many migrants, unable to pay, discontinued treatment; only nine of 68 uninsured migrants continued treatment. The low HIV/AIDS ratio – 2.13 for foreign nationals compared to 2.65 for Japanese nationals for new cases in 2007 – also suggests late detection; the disease is more likely to have progressed to AIDS by the time migrants are tested (39). Instead of providing care, many hospitals urge uninsured patients to repatriate despite grave symptoms. This practice delays essential care and results in poor prognoses; seven of 13 Thai patients diagnosed with AIDS in the latter half of 2004 died before repatriation (41). Last, when HIV/AIDS care is accessed in Japan, it is not necessarily of high quality; a series of studies on HIV+ Latin Americans found that they experience non-supportive doctor-patient relationships and patronization, and that informed consent for treatment is not routinely obtained (15,16).
As for MCH needs, while recent infant mortality statistics are not revealing, the stillbirth incidence for most migrant groups is nearly twice that of the general population (42). MCH access is restricted for overstayer women because they “must decide between possibly jeopardizing their livelihood and existence in Japan or not receiving necessary healthcare for themselves or their children” (14). Fears of being reported to immigration authorities, concerns of cost, and lack of awareness of service availability are all factors that limit access. Indeed, even with NGO support, post-natal checkup and vaccination rates are low (22). As this evidence indicates, disadvantaged migrants, whether categorically excluded from health insurance or otherwise discouraged from enrolling, have unmet healthcare needs.
Advocacy and Policy Solutions
Advocates play a dual role in connecting migrants with care. Advocates create a provisional safety net beyond existing policies and NGO services while simultaneously advocating for change. For example, SHARE and JAR conduct free health consultations and direct patients to hospitals that benefit from, respectively, reimbursement programs and the Free or Reduced Cost Medical Treatment System. JAR also engages municipalities to enroll asylum-seekers in NHI because they reside in Japan for over one year and consequently meet the duration-of-stay requirements. Other organizations, such as SHARE and MIC Kanagawa in Tokyo, Kyoto Multicultural Center in Kyoto and Facil in Kobe, dispatch medical interpreters to increase TB treatment adherence and increase access in general. The various NGOs tackle different aspects of migrant healthcare and become well versed in their fields.
Advocates come to understand necessary policy changes through working on individual cases and are keenly aware of the limitations of their activities (8). Most advocates acknowledge that migrant healthcare access is contingent on case-by-case intervention. Hence, advocates also provide local and national policy solutions that would transform rudimentary policies into the basis for a reliable safety net. Many of the advocates envision components of an ideal system in which all residents have health insurance and medical interpretation is provided as medical service, but most efforts are tempered by feasibility considerations. Perhaps as a result of perceived or actual administrative and legislative inflexibility, as discussed below, advocates’ policy solutions do not resemble the policies of Italy, where all residents enjoy relatively equal access to care, but instead focus on the essential services considered here; advocates’ solutions are markedly practical.
Since current policies fail to form an effective safety net, advocates focus on improving healthcare access through strategies that fit within their scope of expertise and ability that seek to strengthen the existing safety net or reduce its necessity. Efforts of advocates who demand enforcement of current policies and establishment of incentives for safety-net providers may fortify the exiting safety net. Generally speaking, advocates seek policy that prohibits the denial of essential care and provides reimbursement to care providers to improve emergency and infectious disease care access (27). As an example of one approach that simultaneously targets local and national administrations and seeks broad changes, SHARE recently began a funded three-year project to establish a “model prefecture” with a reliable safety net, collect data that suggests positive outcomes result and advocate for the expansion of successful policies throughout Japan (31). The “model prefecture” is to have publicly financed medical interpretation, a reimbursement system and migrant-friendly hospitals – in other words, a strong safety net. Ms. Lee provided the reasoning behind this approach: “We want to set a good example and point the economic benefits for the nation, how it is economically effective and good in terms of public health, how it relates to Japan’s international image”.
Various groups also endeavor to strengthen the safety net by targeting specific policies. For example, in response to Thai women being denied HIV/AIDS care, Thai NGOs and SHARE petitioned the MLHW to mandate the provision of necessary HIV/AIDS care. Although no official policy was issued, the MLHW directed local governments in a letter to instruct hospitals to provide necessary urgent care. In the same vein, Ijyuren, a network of migrant-support NGOs that plays a prominent advocacy role, calls on the MLHW to more aggressively extend emergency care to uninsured migrants (27). As for MCH, a prolific activist academic asserts that while current policies formally allow access to basic MCH services, actual access is limited; hence, she suggests creating a central, flexible MCH support system (43). This would likely allow for better enforcement of current policies and thus a more reliable safety net.
As language is a significant barrier to healthcare access, a number of groups work to increase medical interpretation availability and to institutionalize medical interpretation in Japan (34,44,45,46). Shigeno Aguri, Chairperson of the Board of Kyoto Multicultural Center, detailed one pragmatic approach that would have medical interpretation introduced into the medical insurance reimbursement scheme, thereby institutionalizing interpreter services: “people without insurance will get excluded so I don’t think it’s perfect. It’s a step in the right direction though, especially since there is nothing now” (45). Yoshitomi Shizuyo, of Facil Multilanguage Center, believes that a government budget for medical interpretation is essential and “once it is in the reimbursement scheme, the medical institutions will start to recognize it as a necessary service. It will become part of medical consciousness that interpretation is a fundamental medical service” (44). Facil has worked towards this goal by inviting government officials to panels during which hospitals describe their experiences with medical interpretation. The Kyoto Multicultural Center also involves the local government, their funding source, in collaboration. Matsunobe Megumi, a leader at MIC Kanagawa – an organization that has dispatched interpreters in over 13,000 cases, acknowledged the importance of evidence in advocacy and in the value of “putting together data that show that if there is a proper medical interpreter system and other things like health consultations, then TB and HIV/AIDS cases may go down, which has cost-effectiveness implications” (46). Collectively, advocacy regarding medical interpretation is step-wise and sensitive to the notion that while immediate and complete reform may be infeasible, expanding services is crucial because language barriers limit access regardless of safety-net integrity.
In addition to efforts to strengthen the safety net, advocacy solutions also seek to reduce safety-net dependence by increasing insurance enrollment through changing key features of NHI and EHI policy. A persistent group in Hamamatsu repeatedly petitioned the local government and the MLHW to accept all residents into NHI, but both were unresponsive (9). Similarly, for asylum-seekers, JAR lobbies the MLHW to officially allow asylum-seekers on three-month visas to enroll in NHI. Sakurai Mika, the chief Protection and Assistance Unit Social Assistance Officer at JAR, described their advocacy goals: “Of course, we would like everyone included [in health insurance], but we’re prioritizing our advocacy for people with the three-month visa…which is restricted to people who enter the country legally on short-term visas”. She asserted that ideally all overstaying asylum-seekers would be allowed to enroll in health insurance, but “that sort of stance is hard to have accepted…that would be the next step in a step-by-step process” (17). Thus far, the MLHW response has been lukewarm, merely informing JAR that it is permissible for asylum-seekers on special three-month visas to enroll in NHI. As the collective voice of migrant advocates, Ijyuren annually recommends allowing uninsured migrants, regardless of visa status, to enroll in NHI (27). Though it is important to advocate these comprehensive reforms of fundamental policies, significant change is not expected, especially given pending policies that further restrict access for some migrants; so, fine-tuning the safety net through policy solutions that seeks to strengthen the safety net remains vital.
Discussion
Despite the availability of well-informed policy solutions, the MLHW plans changes that will further disenfranchise uninsured migrants. All legal migrants will tentatively receive a “resident” card from the Ministry of Justice’s Immigration Bureau that enables access to social services, including health insurance (47). Additionally, starting in 2010, visa renewal will require insurance enrollment (48). These developments will likely reduce safety-net dependence for legal migrants as more would be enrolled in NHI and EHI. However, the new migrant control policy threatens to make overstayers invisible; healthcare access for this vulnerable population will decrease as insurance enrollment, once at the discretion of municipal governments, will now effectively be under the domain of the Ministry of Justice Immigration Bureau, which controls who receives a “resident” card. Currently, even an overstayer can update his/her foreigner registration card at the local government office, and at the discretion of the office, be enrolled in NHI if the duration of residence exceeds one year. The Immigration Bureau, true to its purpose, will effectively serve as a gate keeper, denying overstayers a “resident” card and thus denying access to all government services. In light of planned changes, advocates play a particularly vital role in offering solutions to strengthen the safety net for those without access to mainstream health services.
That being said, MLHW policy has not substantially improved since 2000, when it officially expanded access to MCH. MLHW responses to 20 years of advocacy have been categorically inflexible; advocates are only successful when their objectives align with those of the bureaucracy or their efforts are buttressed by international pressure (49,50). Even after expanding access to MCH for overstayers in 1995, the MLHW refused to explicitly inform local governments of this change, arguing, “Overstayers are people we expect not to exist in Japan, right? Wouldn’t it be strange if we issued information that pertains to people that we don’t expect to exist within Japan?” (21). Current efforts face the same fate: MLHW policy stagnates while some local governments have taken necessary action, by, for example, establishing limited reimbursement programs.
Advocates attribute policy inflexibility to various factors, many of which also constitute the constraining political atmosphere that understandably tempers advocates’ policy solutions. As described, many advocates reference ideal policies but advocate those that they consider feasible. Ms. Lee did exactly this: “It would be most ideal to, like other countries, give free health care to all people. That would reduce the burden on the hospitals, but there are many obstacles to realizing this. So, if that were unsuccessful, the second most ideal solution is a reimbursement system” (34). One recurring theme in interviewees’ explanations of modest advocacy was the notion that the lack of political representation of migrants impedes reform. Ms. Lee, a non-naturalized, multi-generation zainichi resident herself, stressed both aspects of the issue in asserting, “There really aren’t any politicians who are interested in the non-Japanese. Non-Japanese people don’t have suffrage. Even I don’t have suffrage…Politicians don’t benefit in any way from helping those who don’t have suffrage”. Migrants cannot exert influence over legislators, and, more importantly, migrants’ needs receive minimal to no consideration in the Diet. In reference to the medical interpreter issue, Ms. Yoshitomi noted, “I have yet to see a Diet member mention the issue” (44). Leny Tolentino, a Filipina who serves as a lay missionary and coordinator of the Women’s Project at the KALAKASAN Migrant Women Empowerment Center, expressed the same frustration: “They don’t seem to hear what the NGOs and the migrants themselves are saying – this is the big obstacle. It doesn’t seem to connect. Unless there are some policy-makers, administrators who really have ears to listen, it will be difficult…” (51). Advocates are aware of, if not frustrated by, their inadequate direct and indirect influence on policy.
A number of advocates also alluded to the broader cultural and historical context of immigration and related policy to explain the MLHW’s inflexibility. Ms. Shigeno, of the Kyoto Multicultural Center, addressed the exclusivity inherent in Japanese immigration policy. “Japanese people think that foreigners will leave at some point, so there isn’t a legal basis for thinking of foreigners as residents” (45). As commentators have detailed, Japanese immigration and related policy draws on misguided sentiments of Japanese homogeneity while pandering to the labor needs of the nation; it officially prohibits the existence of foreign unskilled laborers in Japan while securing their flow through, for example, the Nikkeijin and trainee policies (52). The resulting migrant policies thus serve to control immigration without addressing the reality that migrants become residents and have social needs. Mr. Takayama offered this very explanation when asked about the slow pace of change: “It’s a fundamental problem. Japan is trying to get illegal people to leave and trying to think of ways to get people to come legally to Japan and work” (21). Mr. Inaba of Africa Japan Forum put this policy dynamic in historical perspective: “Exclusive immigration policy is a fundamental policy of post-war Japan” because “There is this system with the emperor and the Japanese blood-base, which is the unwritten context of today” (35). Indeed, it may prove fruitful to examine Japanese migrant policy with an eye towards the nihonjinron phenomenon, which emphasizes Japanese uniqueness and homogeneity. It is in this context that, as Ms. Lee maintained, the flexibility of interpreting “kokumin” as “citizen,” instead of as “people,” in Article 25 of the Japanese constitution allows for the exclusion of many migrants from the social welfare, security and public health privileges that are otherwise guaranteed to kokumin (34). In this environment, then, it is hardly surprising that the efforts of advocates are slow to bring change.
Importantly, however, advocates’ policy solutions are consistent with international precedent. As a signee of the International Covenant on Economic, Social and Cultural Rights, Convention on the Elimination of All Forms of Racial Discrimination, Convention on the Elimination of All Forms of Discrimination against Women and Convention on the Rights of the Child, Japan should guarantee access to essential health care and MCH to all residents. As described, while EU member states represent diverse policies, most guarantee access to emergency care and many provide for MCH and infectious diseases care, including care for HIV/AIDS, to all residents including undocumented migrants and asylum-seekers. Most of these nations extend care to all residents by reimbursing providers that act as safety nets (5). Japanese advocates’ pressure to increase access to emergency, infectious disease and MCH for all residents and to increase funds for providers is hence congruous with policies of other developed nations.
While many EU nations do extend varying levels of healthcare to all migrants, recent years have seen some increasing restrictions. Italy is lauded for its migrant-friendly system, but Italian lawmakers, attributing law and order problems to the growing undocumented migrant population, recently considered legislation requiring undocumented migrants to pay the full cost of care and also to allow physicians to report undocumented migrants to the authorities (6,53). Similarly, England, concerned about alleged abuse of its migrant-friendly policies and the alleged “health tourism” phenomenon, passed legislation in 2004 to limit undocumented migrants’ health care access and may pass more similarly restrictive legislation (5,54). The HUMA report regarding migrant healthcare in 10 European countries summarizes recent restrictive legislation and concludes that there is a “generalized tendency in all EU countries to restrict undocumented migrants’ entitlements to access health care and to look at health as an instrument serving immigration control purposes” (5). Germany, however, may make it possible for undocumented migrants to access certain care anonymously, thus eliminating one deterrent to care. Hence, it appears that policy-makers in the EU are struggling to strike a balance between controlling immigration and providing adequate healthcare. The pending Japanese policies evidence a similar struggle in the Japanese context.
In terms of additional challenges to healthcare safety nets, the United States’ safety-net is threatened by the increased demand and decreased funding that characterizes the economic recession. An examination of the American case noted that safety-net providers are highly dependent on two entitlement programs – Medicare and Medicaid – and as state budgets have decreased and demand increased, financial resources have been stretched thin (55). Given the high cost of care, “Health care providers increasingly refuse to care for patients who are covered by safety-net programs because they consider the reimbursement levels too low” (56). This background contextualizes Dr. Sawada’s assertion that, in addition to disadvantaged migrants, Japanese “working poor and people without health insurance are having a hard time getting care, too” as a result of Koizumi administration policy changes that pressure hospitals to be financially successful (23). Ms. Matsunobe of MIC Kanagawa also suggested that Koizumi administration policy is an obstacle in the way of policy change regarding medical interpretation services: “I think the entire Koizumi administration (2001-2006) is bad. Medical costs are going up so they’re trying to reduce costs” (46). In summary, while advocates’ policy solutions are consistent with precedent and in line with various international conventions, their efforts are impeded by challenges that are hardly unique to the Japanese migrant healthcare situation; financial constraints, in addition to concerns of immigration control, likely discourage policy-makers from welcoming migrant-friendly reform.
Nonetheless, when uninsured, disadvantaged migrants in Japan unequivocally face limited access to essential healthcare and experience relatively poor health. Healthcare access can be improved by facilitating enrollment in health insurance, but this is a valid solution only for eligible migrants. A healthcare safety net is necessary for migrants who currently are and will be denied access by pending reform and for eligible but uninsured migrants. A few policies currently form a provisional safety net, but these limited policies are weakly enforced and safety-net providers are few. Additionally, the absence of policy that guarantees access to urgent care essentially allows providers to prioritize financial concerns. This combination of weakly enforced policies, policies rendered ineffective by various limitations and the absence of guaranteed access to urgent care produces an ineffective safety net. Faced with a safety net that fails to meet migrants’ needs, advocates offer policy solutions to remedy said weaknesses. While advocates are generally optimistic and believe that gradual change is possible, twenty years of advocacy has resulted in limited change; their policy solutions are thus modest and focus more on stepwise strengthening of the safety net and less on fundamental health policy change. As Japan faces increased pressures to accept immigration in response to its demographic shift, the importance of advocates’ solutions cannot be dismissed. How Japan ultimately balances immigration control and migrant rights and how it responds to migrant health needs in the context of financial limitations – whether through establishing an all-inclusive health insurance system or transforming the current patchwork safety net into a reliable one – will interest policy-makers and advocates in established migrant-receiving countries and in other Asian nations such as South Korea that are dealing with comparable immigration issues.
Acknowledgements
The author would like to thank Kashiwazaki Chikako at Keio University for advocate contacts, research advice and manuscript comments, Edson Urano at Sophia University for advocate contacts and research advice and SHARE-Tokyo for allowing me to serve as an intern and for putting me in contact with various NGO leaders.
Neal S. Parikh served as an intern of the domestic section of SHARE, an established Tokyo NGO that has long been involved in migrant health care, for seven months to obtain a firsthand understanding of disadvantaged migrant healthcare in Japan. He wrote this article for The Asia-Pacific Journal.
Recommended citation: Neal S. Parikh, “Migrant Health in Japan: Safety-Net Policies and Advocates’ Policy Solutions,” The Asia-Pacific Journal, 12-3-10, March 22, 2010.
See the following articles on related themes
Hiratate Hideaki, Patients Adrift: The Elderly and Japan’s Life-Threatening Health Reforms
John Creighton Campbell, The Health of Japan’s Medical Care System: “Patients Adrift?”
Notes
1 The author systematically searched the Igaku-chuo-zasshi (Japana Centra Revuo Medicina) Japanese-language medical literature database for research regarding migrant health. Additionally, the author interviewed thirteen representatives of established migrant-support NGOs in Tokyo, Kyoto and Kobe. Interviewees included NGO leaders, key staff, physicians, and advocates. Interviews centered on migrant health, access barriers, limits of non-advocacy activities, policy solutions, and advocacy efforts. The author also collected unpublished organizational data and in-house publications.
2 “Disadvantaged migrants,” as used in this discussion, refers to those migrants with immigration statuses with limited privileges; the migrants of particular concern are those with limited working privileges and limited access to welfare systems. Included in this category, in addition to those explicitly mentioned, are sex workers who have entered Japan on entertainer visas, tourist visas and through other mechanisms. This discussion excludes the zainichi population of resident Korean and Chinese; most zainichi individuals are second, third or fourth generation, are variably integrated into Japanese society, and have the option to naturalize and thus receive rights equal to those of Japanese citizens. This discussion also excludes “advantaged migrants” like those from America, Europe and India who reside in Japan transiently for work in business, technology, education and so on.
References
1 Bollini P, Siem H. No Real Progress Towards Equity: Health of Migrants and Ethnic Minorities on the Eve of the Year 2000. Soc Sci Med. 1995:41(6):819-828.
2 Derose KP, Escarce JJ, Lurie N. Immigrants and Healthcare: Sources of Vulnerability. Health Affairs. 2007:26(5):1258-1268.
3 Institute of Medicine. America’s Healthcare Safety Net: Intact but Endangered. Washington: National Academies Press; 2000.
4 Romero-Ortuño R. Access to healthcare for illegal immigrants in the EU: should we be concerned? European Journal Health Law. 2004:11:245-272.
5 PICUM. Access to Health Care for Undocumented Migrants in Europe. Brussels, 2007. Available here, accessed 10 April 2009.
6 HUMA network. Access to Health Care for Undocumented Migrants and Asylum Seekers in 10 EU Countries: Law and Practice. 2009. Available here, accessed 10 March 2010.
7 Scott P. Undocumented Migrants in Germany and Britain: The Human “Rights” and Wrongs” Regarding Access to Health Care. Electronic Journal of Sociology. 2004. Available here, accessed 10 March 2010.
8 Ministry of Justice. Gaikokujin toukei. Available here, accessed 13 May 2009.
9 Yamanaka K. Migration, differential access to health services and civil society’s response in Japan. In: Jatrana S, Toyota M, Yeoh BSA, editors. Migration and Health in Asia. New York: Routledge; 2005. p.141-160.
10 CARAM Asia. State of Health of Migrants 2005. Kuala Lumpur: Caram Asia Berhad; 2006.
11 Shipper AW. Fighting for Foreigners. Ithaca: Cornell University Press; 2008.
12 Sellek Y. Migrant Labour in Japan. New York: Palgrave Macmillan; 2001.
13 Stevens C, Lee S. Reproducing identity: maternal and child healthcare for foreigners in Japan. In: Goodman R, editor. Family and Social Policy in Japan. Cambridge: Cambridge University Press; 2002. p.92-110.
14 Stevens C, Lee S, Sawada T. Undocumented Migrant Maternal and Child Healthcare in Yokohama. Journal of Japanese Studies. 2000:20(1):49-65.
15 Castro-Vázquez G, Tarui M. Embodiment and Sexual Experiences of Some Latin American PLWHA Men in Japan. Sexuality & Culture. 2006:10(4):81-113.
16 Castro-Vázquez G, Tarui M. A Service Or a Right Informed Consent for HIV-Positive Latin American Men in Japan. Anthropology & Medicine. 2007:14(2):197-212.
17 Interview: Mika Sakurai (Japan Association for Refugees). 2009 Apr 28.
18 Ministry of Justice. Honpou ni okeru fuhouzanryuushyasuu ni tsuite Heisei 21 ichigatsu tsuitachi genzai. Available here, accessed 7 May 2009.
19 Ministry of Justice. Heisei 20nen ni okeru nanminninteishyasuu nado ni tsuite. Available here, accessed 17 May 2009.
20 Kojima H. Foreign Workers and Health Insurance in Japan: The Case of Japanese Brazilians. Japanese Journal of Population. 2006:4(1):78-92.
21 Interview: Takayama Toshio (Himawari Clinic, Solidarity Network with Migrants Japan). 2009 Apr 30.
22 NGO ni yoru kobetsushisetsusou no shien to sono hyoka ni kansuru kenkyuu, editor. Iryousoudanin no gaikokujin HIV youseishya ryouyou shien handobukku. Tokyo: SHARE; 2007.
23 Interview: Takashi Sawada (Minatomachi Medical Center, SHARE). 2009 Apr 16.
24 Interview: Catherine Campbell (National Union of General Workers Tokyo Nambu). 2009 May 15.
25 Watanabe Y. Zairyuushikaku ganai zainichigaikokujin he no boshihoken saabisu. Japanese Journal Pediatric Medicine. 2005:37(3):392-396.
26 Shimoto I. Zairyuushikaku ni kakawarazu riyou dekiru “muryou teigaku shinryou seido”. In: Network for Medical Care and Life of Migrant Workers, editor. Gaikokujin no iryou to fukusi – NGO no jissen jirei ni manabu – . Tokyo: Ijyuren; 2006. p.36-39.
27 Seido riyou ni atatte no adobaisu. In: Network for Medical Care and Life of Migrant Workers, editor. Gaikokujin no iryou to fukushi – NGO no jissen jirei ni manabu –. Tokyo: Ijyuren; 2006. p.103-125.
28 Nakamura Y. Zainichigaikokujin no tame no yobou sessyu. Journal of Ped Practice. 2004:67(11):2079-2085.
29 Solidarity Network with Migrants Japan. Taminzoku/tabunka kyousei shyakai no kore kara – NGO kara no seisaku teigen. Tokyo: Solidarity Network with Migrants Japan; 2009.
30 Interview: Murayama Satoshi (Kanagawa City Union). 2009 Mar 26.
31 Yamamura J. A Study on Free Medical Check-ups for Foreign Workers. In: Minatomachi Foreign Migrant Workers’ Mutual Aid Scheme for Health, editor. MF-MASH minatomachi kenkou taijyoukai shiryousyuu. Tokyo: 2002. p.62-74.
32 Azeyanagai Y, Mizuguchi M, Shibasaki A, Uchisaka Y, Matsumura T, Tashiro M. Naganoken ni okeru gaikokujin kenshinjyushinshya no kenkou jyoutai to kongo no kenshin no arikata – NGO shyusai ni yoru gaikokujinkenshin no kekka bunseki yori – . Bull Nagano Coll Nurs. 2008:10:101-112.
33 AIDS Groups Besiege Japanese PM. The Nation [Internet]. 2008 Jul 31 [cited 2009 Apr 7];National:[about 1 screen]. Available here.
34 Interview: Lee Sangnim (SHARE). 2009 Apr 15.
35 Interview: Inaba Masaki (Africa Japan Forum). 2009 Mar 3.
36 Ministry of Health, Labour and Welfare. Heisei 19nendo kekkaku hassei doukou chyousa nenhou shyuukei kekka. Available here, accessed 13 Mar 2009.
37 Shirakuoka C, Oomori S, Takao R, Yamada M, Muroi M, Nagamine M, et. al. Shinjukuku hokenjyo ni okeru kekkaku taisaku. Kekkaku. 2008:83(9):611-620.
38 Interview: Matsunobe Megumi (MIC Kanagawa). 2009 Feb 27.
39 Kouseiroudoushyou toukeihyou deetabeesu sisutemu [Internet]. Dai 2-10hyou, HIVkansenshyasuu/AIDS kanjyasuu, kokusekiXkansenkeiro-sei-kansenchibetsu;[cited 2009 May 3];[about 1 screen]. Available here in Japanese.
40 Sawada T. Gaikokujin HIV kansenshya no chiryou kankyou to shien. Progress in Medicine. 2003:23(9):2313-2316.
41 Sawada T. International Society is Trying to Promote Access to Treatment: Expected role of Local Government in Responding to HIV. Journal National Institute of Public Health. 2007:56(3):253-256.
42 Ministry of Health, Labour and Welfare. Heisei 19 jinkou doutai toukei. Available here, accessed 23 Apr 2009.
43 Ri S. Tabunka kyousei jidai ni motomerareru boshihoken. Japanese Journal for Public Health Nurse. 2006:62(12):996-999.
44 Interview: Yoshitomi Shizuyo (Facil Multilanguage Center). 2009 Mar 22.
45 Interview: Shigeno Aguri (Kyoto Multicultural Center). 2009 Mar 13.
46 Interview: Matsunobe Megumi (MIC Kanagawa). 2009 Feb 27.
47 Matsutani M. Immigration reforms spell Big Brother, JFBA warns. Japan Times [Internet]. 2009 March 26 [cited 2009 May 27];News:[about 2 p.]. Available here.
48 Ministry of Justice Immigration Bureau. Zairyuushikaku no henkou, zairyuu kikan no henshinkyouka no gaidorain. Available here, accessed 2009 May 15.
49 Milly DJ. Policy Advocacy for Foreign Residents in Japan. In: Takeyuki T, editor. Local Citizenship in Recent Countries of Immigration: Japan in Comparative Perspective. Oxford: Lexington Books; 2006. p.123-152.
50 Gurowitz A. Looking Outward: International Legal Norms and Foreign Residents in Japan. In: Takeyuki T, editor. Local Citizenship in Recent Countries of Immigration: Japan in Comparative Perspective. Oxford: Lexington Books; 2006. p.153-170.
51 Interview: Leny Tolentino (KALAKASAN Migrant Women Empowerment Center). 2009 Mar 9.
52 Tsuda T, Cornelius W. Japan: Government Policy, Immigrant Reality. In: Cornelius W, Tsuda T, Hollifield J, Martin P, editors. Controlling Immigration: A Global Perspective. Second Edition. Stanford: Stanford University Press; 2004. p.439-476.
53 Squires N. Italian doctors forced to report illegal immigrants. Telegraph [Internet]. 2009 Feb 5 [cited 10 March 2010];News;[about 1 p.]. Available here.
54 Belluz J. UK migrants: ‘Leaving the hospital felt like walking my father to his death’. The Times [Internet]. 2008 Dec 8. [cited 10 March 2010];Health;[about 4 p.]. Available here.
55 Lewin ME, Baxter RJ. America’s Health Care Safety Net: Revisiting the 2000 IOM Report. Health Affairs. 2007:26(5):1490-1494.
56 Redlener I, Grant R. America’s Safety Net and Health Care Reform – What Lies Ahead? NEJM. 2009:361(123):2201-2204.