By Yabuki Toshihito
Translated by Nobuko ADACHI
Some say that these days Japan is entering “the new era of heath care deterioration.” The current government has just rammed through the Diet the Medical Care Reform Act, which drastically curtails spending on hospitalization insurance and medical care for the elderly. This regressive revision of the health care insurance law most directly affects older people. What is going to happen to people who need hospitalization or long-term care? What kind of medical care can the elderly now expect to receive?
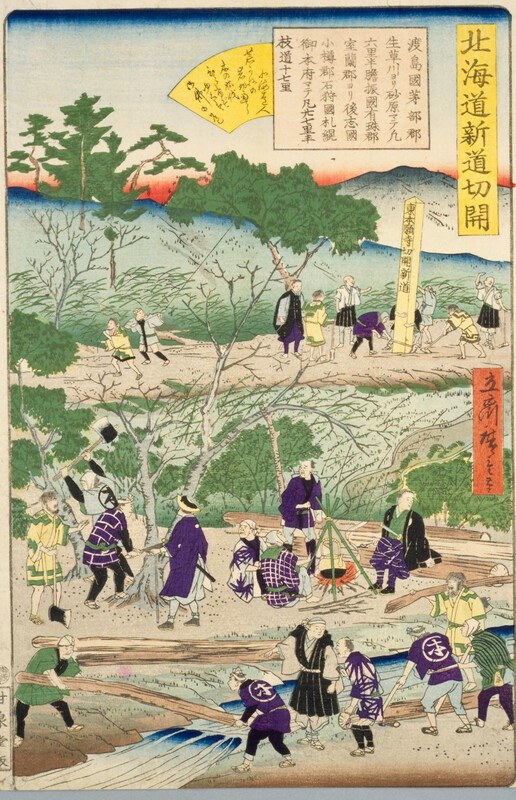
The population of Nemuro City in Hokkaido is about 31,000. Because of the continued decline of the fishing industry—the economic backbone of the area—the population of the city has rapidly decreased and those who remain are largely the elderly and the aging. The Community Welfare Clinic of Nemuro City Hospital was the only institution providing long-term care beds in the city. This February, however, the owner of the clinic announced at a press conference that, “After the new insurance reform law was passed regarding care for the elderly, the hospital has lost a great number of patients, so we will have to eliminate long-term care services. It is impossible to operate under these conditions.” One month later, the whole clinic was closed.
Suzuki Toshihiro (56), whose 83 year-old father was a patient at the clinic, was stunned. His father had been treated there since last July, and in April was planning to move to the long-term care wing. “My father used to live with my mother and my brother. However, my brother became a diabetic and my mother died of colon cancer, so I gave up my job and returned home to take care of him. Because my father had a stroke and suffers from Parkinson’s, he needs full-time care.”
Toshihiro’s father got the flu last July and was hospitalized in Nemuro City Hospital. But even after recovering from the flu he could not talk, and lost the use of his limbs. Fortunately, he was slated to receive long-term care, and Toshihiro planned to return to work. Then suddenly the closure of the clinic was announced. “The other institutions they suggested I go to that take public aid were all located over two hours away by car. Not only was the distance a problem, but all patients had to leave these institutions after several months. As a result my father had to return home. Because I have to look after him, I gave up trying to find full-time work. At the Nemuro Community Welfare Clinic, he could have been looked after for the rest of his life.”
Today Toshihiro tries to get by taking part-time work while looking after his father. He says, “A family member suffers most when someone has health problems. It is hell.”
As for the patients who lost long-term care services …
At the time when the Community-Welfare Clinic of Nemuro City Hospital was closed, there were fifty-seven patients in residence. Suzuki Yoshiko and Kubo Michiko—a nurse and professional caretaker at the hospital, respectively—blame the clinic management for its demise. “Even in the meeting they had with the patients’ families, they simply made excuses instead of trying to offer any financial solutions, and told everyone to just find a new hospital,” Suzuki commented.
According to Suzuki, only twenty-one out of fifty-seven patients could find other medical institutions. Fourteen patients had to move in with their families at home, some of them moving all the way to Tokyo. Five passed away within three months of leaving the hospital, probably because of these drastic lifestyles changes.
Sasaki Fumie (68), who came to the hospital in mid-January, had to return home after only a very short stay. Her husband explained, “My wife had been bedridden at home with rheumatism, but when she developed an ulcer she was hospitalized in the city hospital. Six months later, we were asked to leave. We finally found the Community-Welfare Clinic of Nemuro Hospital. I had hoped she could continue rehabilitation there until she got well enough to go to a nursing home.”
Her husband—who is now providing for all her care—had to discontinue treatment for his own health problems. Because he was in a car accident he ruptured a vertebra, and now has a herniated disc in his back. He suffers from numbness in both hands and feet. “Since I am the only one around, however, I have to look after her all by myself. I prepare meals for her and change her diapers. But if something happens to me, then both of us are finished.”
Until now Nemuro City had managed to take care of its elderly by providing health care through Nemuro City Hospital, the Community-Welfare Clinic, and individual family doctors. This year five internists who were sent by the University Hospital to the City Hospital were removed because of budget cuts at the university. This shortage of physicians, together with the closing of the Community-Welfare Clinic, precipitated the current local health care crisis.
Shimatani Mitsuru, the chief of the Department of Welfare and Insurance at Nemuro City Hall, comments that “ In this locality, where the population is rapidly aging, we find that when patients have to be treated at home, it is often the elderly looking after the elderly. Without recognizing this reality, the government defines public hospitalization as a bad thing, and discontinues long-term care services.”
Who are the targets of these medical care budget cuts?
The situation in Nemuro City is not at all a “local” social problem. According to changes in the medical security law passed last June, the government will cut sixty percent of the long-term care budget over the next six years. This means that the current 380,000 beds the country now provides for long-term care will be cut to 152,000.
Tsukiji Hiroshi lives in Tokyo’s Chiyoda Ward. He has a 74 year-old uncle, who was ordered to leave a long-term care center this May. His uncle was told by the director that “We are asking all of our patients to leave the hospital, except those who need dialysis or are facing the final stages of a fatal disease. We are even asking those who are on feeding tubes to leave.”
The uncle, who was hospitalized at a university hospital last October for congestive heart failure, was asked to leave after just thirty days. He found a rehabilitation clinic near his home. But he was soon asked to leave even from there.
Hiroshi said, “Later he finally found another rehabilitation clinic, but the monthly fee is 420,000 yen. Since his social security pension cannot cover the fee, he worries constantly about his finances.”
Dr. Matsuda Masao, a vice president of Mitsuya Hospital in Ishikawa Prefecture and member of the board of admissions of the Rehabilitation Hospital Association, has serious doubts about current welfare policies.
“The Ministry of Welfare and Labor divides patients into three categories depending upon the degree of healthcare needs. Those who are least in need, classified as Category 1, are candidates for treatment at home.”
Included in this category, however, are people with some serious problems, such as someone who is “a terminal cancer patient who is not in pain, but needs to be fed intravenously once or twice a day” or “a patient who cannot swallow food because of a tracheotomy which must be cleaned up to seven times a day.”
Dr. Matsuda says these patients have been classified in the least-need category because the Ministry of Welfare and Labor stipulated that at least fifty percent of all rehabilitation patients be in Category 1. Now, in Category 3 are people who generally are allowed long-term hospitalization. However, some in Category 3 have short-term problems, such as those who need 24 hour supervision, or who require temporary quarantining for a contagious disease.
Dr. Matsuda warns that “the Ministry will be trying to cut budgets greatly over the next twenty years. This means that it is the baby-boomers who will be directly affected. They need to recognize this situation immediately, and to protest it.”
Have we produced a system of “discriminatory medical care”?
Twenty-one social workers from five medical corporations belonging to the Nagano Prefectural Association of Democratic Medical Institutions have been investigating why some people are unable to receive adequate health care.
“Every year we investigate about 150 cases. The reasons we used to hear for why people lost their health care coverage were things like ‘I lost my job due to risutora [economic restructuring leading to firing employees] and became homeless,’ or ‘After the firm collapsed I had to live in my car or on the street, getting water at a park.’ But recently we are hearing not only about such extreme cases, but more and more cases of ordinary people having problems.”
Oneinvestigator, Ayukawa Yukari, told me of some of her cases. For example,
• A woman in her late 60s: She was stricken with cerebral thrombosis. Her husband worked at a news agency and her daughter in her thirties also had a decent job. However, the daughter became depressed while looking after her mother. The family was not able to pay the sudden high costs of the mother’s medical treatments, so they had to pay in installments. But while trying to work this out, the daughter’s depression worsened and she was hospitalized.
• A woman in her early 60s: Her husband was an alcoholic and was being treated at home. The woman lived with her husband and her 28 year-old son who was mentally handicapped. She supported the family through work as a janitor. But having failed to pay the fee for national health insurance, she could not go to see a doctor. Finally, in great pain, she went to see a doctor. By this time she was already in the terminal stages of uterine cancer. She died two months later.
“This woman had gone to City Hall to ask about her financial options. Although he knew her son was mentally handicapped, the official advised that the son should get a job. If he had treated her more humanely she could have been treated for her cancer earlier.”
Koike Akira, a Communist Party Diet member, laments that such medical care “boat-people” are seen all over Japan today.
“Five years ago the Koizumi government broke an unwritten rule about having a humane health care policy, a promise which not even the Liberal Democratic Party had broken. However, the Koizumi government’s so-called Supporting Cost System actually destroyed the welfare system, and shifted health care costs to those least able to afford it. This government changed the law to take things away from people in ways that would never have even been considered previously.”
Furthermore, Koike says, these reforms are “an affront to the spirit of the Constitution.” “What they did was to cut older people out of the health care system. They also prohibited the combined use of insurance and free medical clinics. I wonder what kind of society we will have as this ‘medical discrimination’ grows?” That is, Japan is rapidly becoming a society where people who have money get priority over health care “boat people” when receiving medical treatment.
More people are dying alone
From late 2005 to March 2006, seven people died alone at the Hiroo Tokyo Subsidized Apartment Complex, which contains 700 units. Why did they die alone in a place that offers convenient public transportation and is close to Tokyo Prefecture Public Hospital?
“These deaths happened one after another. One day we found two bodies, and later we found a body of someone who already had been dead two weeks. All these people were alone, but were seeing medical doctors,” said Nino Kazunori, the 78 year-old chairman of the subsidized-apartment resident’s association. He added, “Before that, a sixty five year old person starved to death. Actually, about ten people starve to death every year.”
It appears that dying alone and hungry is becoming almost a daily event at subsidized housing residences.
Numata Seiichi, 64, lives in a subsidized apartment and has been receiving dialysis for the last nine years. “For almost three years I have had to pay for much of my medicine, depending on the prescriptions, and fees for treatment. My pension is a little less than 90,000 yen ($820), so after paying the rent and medical bills, I have just a little over 40,000 yen left. I can barely eat on that. If something happens, I could not support myself. Many people who live here think that if they ever are hospitalized, that’s the end—it’s time to die.”
Some public housing complexes have started to look after the health and safety of their residents by themselves, since they cannot depend on the government under current welfare and medical care policies. The Komemoto Housing Complex in Yachiyo City, Chiba Prefecture, consists of 3,000 units, and is home to 63,000 people. This complex opened 35 years ago. Currently 983 people are over 65 years old and 180 people live alone. The Resident’s Association organizes activities like a neighborhood-watch network which checks up on the elderly.
“We started this around the time when more and more elderly people were dying alone. The first time this happened, a 70-year old man opened his neighbor’s door, feeling something was wrong. He found his neighbor dead, his body covered with flies. Things like this are just sad. Although we had lived in the same apartment complex, nobody knew about this death,” explained Kato Shiro, the 64 year chairman of the resident’s association. He then showed me a chart of the number of people who die alone each year in the housing complex. At Komemoto, six people died alone three years ago, when they first started keeping track. Since then there have been five or six such cases every year. There have been four already as of March of this year.
“When we go into the apartments of those who died alone—most over the age of 70—we find collection notices all over. They say if you do not pay your gas or electricity bills, they will soon be shut off. I have no way of knowing the immediate cause of their deaths, but I cannot help thinking that they died with no way out,” Kato says with a sigh. “I wonder what the government thinks of these social conditions?” He left to make his rounds with Soeda Masuko, 62 years old, an officer of the resident’s association.
Elderly people who have been cut off from medical care and rehabilitation are moaning in loneliness. The deterioration of our heath care system has already become a reality.
Yabuki Toshihito is a reporter. This article appeared in Shukan Kinyobi July 28, 2006. Posted at Japan Focus September 13, 2006.
Translated for Japan Focus by Nobuko Adachi, assistant professor of anthropology, Illinois State University and editor of Japanese Diasporas: Unsung Pasts, Conflicting Presents, and Uncertain Futures.