Donor Leverage and Access to Bird Flu Vaccines: a challenge to the World Health Organization
CHAN Chee Khoon and Gilles de Wildt
Shifting Alignments in International Health?
In early 2007, the Indonesian government decided to withhold its bird flu virus samples from the World Health Organisation’s collaborating centres pending a new global mechanism for virus sharing that offered better terms for developing countries. In breaking with the existing practice of freely sending flu virus samples to these laboratories, Indonesia expressed dissatisfaction with a system which obliged WHO member states to share virus samples with WHO’s collaborating centres, but which lacked mechanisms for equitable sharing of benefits, most importantly, affordable vaccines developed from these viral source materials.

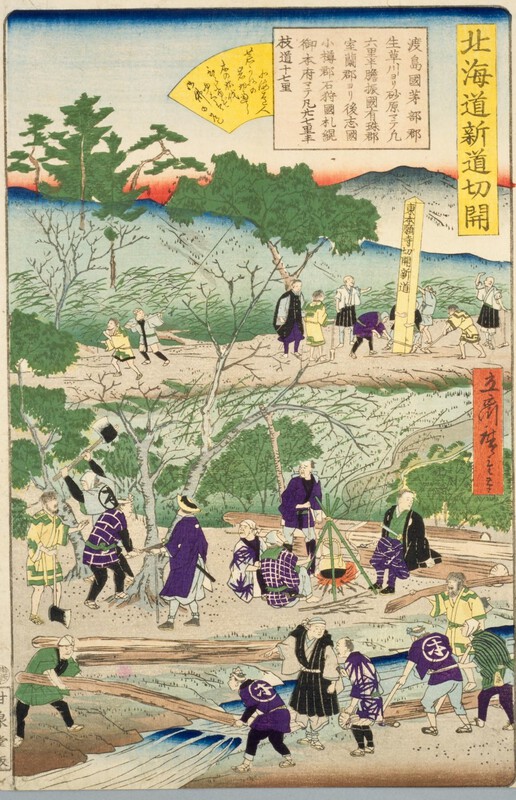
A victim of bird flu is treated at a hospital in
Six other members of his extended family have died from the virus.
The Indonesian decision elicited unease, but also support and sympathy, including an editorial from the Lancet:
“To protect the global population, 6.2 billion doses of pandemic vaccine will be needed, but current manufacturing capacity can only produce 500 million doses. Indonesia fears that vaccines produced from their viruses via the WHO system will not be affordable to them. The fairest way forward would be for WHO to seek an international agreement that would ensure that developing countries have equal access to a pandemic vaccine, at an affordable price.”
In March 2007, following an interim agreement for
The Indonesian government’s stance in particular was notable on three counts:
· it was explicitly a critique of WHO’s balance of pragmatism which it felt was overly accommodative of corporate priorities, to the detriment of the health and wellbeing of a key constituency that WHO was mandated to defend, the underserved communities among its member states
· it was an exercise of leverage by a source country of biological materials seeking to redress the inequities of access to what may be vitally important health inputs (avian flu vaccines) developed from these source materials
· it was seeking equitable benefits from commercial developers not just for its nationals but for other communities as well who were likely to be sidelined by commercially-driven product development and distribution systems
Commodification and the Gift Relationship
These developments call to mind The Gift Relationship, a study of blood donation systems in the
With the prevailing (and still tenacious) ethos of neo-liberalism, however, donors of biological materials not surprisingly come to expect a share of the financial gains made possible by their donated materials. John Moore v. The Regents of the University of California (1990), for instance, was a celebrated case of a leukemia patient who underwent surgery in 1976 at the University of California (UC) for removal of his cancerous spleen. UC was later granted a patent for a cell line called “Mo” established from his spleen, which produced valuable cytokines with a long-term commercial value estimated at over $1 billion. Moore filed suit and demanded the return of the cells and control over his body parts, but the California Supreme Court ruled that he was not entitled to any rights to his own cells after they had been removed from his body.
This principle was re-affirmed in the
A neo-liberal environment thus tends to undermine altruistic (gifting) inclinations, encouraging instead pecuniary if not mercenary tendencies among donors who might otherwise be disposed towards voluntarism, communitarian practices and the common good. Bluntly put, “if researchers and their commercial sponsors are going to enrich themselves using my biological samples and personal data, why shouldn’t I get my share of it?”
Reasserting the Public Domain: Between Commons and Commodification
In the 1990s, Rural Advancement Foundation International proposed an international campaign aimed at a formal Declaration of a Global Genetics Commons. Sir John Sulston (2002 Nobel laureate in medicine or physiology) endorsed a very similar idea, which sought a declaration of the human genome as the common heritage of humanity and for its DNA sequences to be off limits to patent claims.
In the event, the idea was shelved, in part due to the realization that even if genomic DNA sequences were not patentable, downstream technologies utilizing these “commons resources” in the “global public domain” could still be subject to intellectual property claims. Was the patenting of body parts and genetic information part and parcel of an unavoidable trend towards the commodification of life forms then?
A middle path — which accepts intellectual property claims on these biological entities, but ensures that these are retained within the public domain (vested, for example, in trustee institutions mandated to equitably serve the public good) — is one option that may be worth exploring.
In 2003,
In similar fashion, intellectual property arising from publicly funded international collaborative research could be vested with an appropriate international public agency, say WHO, to keep the international property rights within the global public domain. WHO could similarly license these patents on a nonexclusive basis for product development so that useful and affordably-priced generics could be produced in a competitive environment. The modest fees that WHO could earn from this non-exclusive licensing could perhaps also yield a small bonus by reducing the dependence of the institution on donor governments (and corporate donors), and hence, expand the latitude for a more independent role in international health policy advice and technical support.
An ASEAN+3 Initiative for Public Goods?
Seen in this context, the Indonesian initiative on new virus sharing arrangements is noteworthy while its exercise of donor leverage may presage a consideration of trusteeships which could serve as public (international or regional) repositories of genetic resources, genomic information, and other biological materials.
Notwithstanding WHO’s mandate to establish an international stockpile of vaccines, the limited vaccine production capacity globally, and the financial requirements for establishing and maintaining a stockpile of adequate size, remain as key concerns.
Dr Margaret Chan, the Director-General of WHO has called for thinking-outside-the-box for an innovative financing scheme for the international stockpile of bird flu vaccines (Reuters,
One proposal for risk management that was floated – since the stockpiled pre-pandemic vaccines have a shelf-life and potential donors might balk at the recurrent costs of continual replenishments – was to use the donated cash resources to buy insurance coverage instead from a willing underwriter. If and when an outbreak of pandemic flu emerged, the financial payout could then be used to bid for existing stocks of pre-pandemic vaccines that had not already been committed, and to make immediate advance purchase orders for supplies of the pandemic strain vaccine. Notwithstanding Dr Chan’s call for bold thinking, this proposal seems entrapped within a market-driven approach which may keep proprietary vaccine manufacturers happy (and insurers, if they were suitably hedged), but would do little in the short run to directly expand vaccine manufacturing capacity in line with the precautionary principle.
Taking Dr Chan’s call to heart, and stepping outside the box of obsessive bias against public enterprises in their roles as manufacturers and providers of public goods, we would extend Kucinich’s proposal to the global arena and call upon WHO to explore the feasibility of an international public enterprise that could produce, acquire, and manage an international stockpile of avian flu vaccines that can be made available as public goods on a rational and transparent priority needs basis.
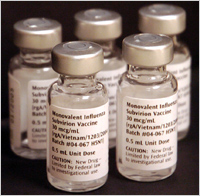
Samples of the Avian Influenza Vaccine, displayed
at the University of Maryland School of
Medicine in
In the meantime, it would be wise to also consider regional initiatives that could be implemented without undue delay within an institutional framework with a functional track record. The 2002-2003 Severe Acute Respiratory Syndrome (SARS) epidemic forcefully demonstrated the regional economic consequences of a life-threatening infectious epidemic, whose effects would be dwarfed by the likely human and economic impacts of highly transmissible and lethal human flu. A persuasive case could therefore be made for an East Asian regional initiative (perhaps ASEAN+3, with their evident concerns over the economic impact of financial contagion in volatile capital markets) to provide the institutional framework for mobilizing the financial and technological resources in the region to enhance regional preparedness in a likely epicentre of a flu pandemic. This would go beyond the existing co-ordination of surveillance networks to include the development or expansion of vaccine manufacturing capabilities to augment regional stockpiles of avian flu vaccines.
Beyond the immediate concern of timely and affordable access to pandemic flu vaccines, the Indonesian initiative has also raised the intriguing possibility of other analogous instances where donors of biological materials and personal data could utilize the leverage of their gift relationship in furtherance of the common good.
CHAN Chee Khoon ([email protected]) is with Universiti Sains
A longer referenced version of this article is available as a UN-DESA working paper. This article was written for